
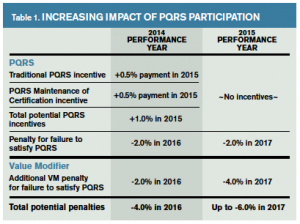
Last fall, the Centers for Medicare & Medicaid Services (CMS) released the 2015 Medicare Physician Fee Schedule Final Rule, which makes significant changes to federal quality reporting requirements and holds physicians to an increasingly high bar. Satisfactory participation in Physician Quality Reporting System (PQRS) becomes especially critical because 2015 marks the official end of PQRS incentive payments as the program transitions to penalties only (see Table 1). The 2015 PQRS reporting year also will determine an additional payment adjustment under the Value Modifier (VM) in 2017, which now applies to all physicians and carries stiffer penalties for large groups.
Explore This Issue
ACEP Now: Vol 34 – No 02 – February 2015In order to avoid the PQRS adjustment, CMS requires eligible professionals to report nine measures across three national quality strategy domains, which must also include at least one “cross-cutting” measure:
- Person- and caregiver-centered experience
- Patient safety
- Communication and care coordination
- Community and population health
- Efficiency and cost reduction
- Effective clinical care
Cross-Cutting Measures
This year, CMS also finalized a newly designated list of cross-cutting measures, which represent a core set of measures that CMS feels addresses critical improvement gaps that apply across specialties. The cross-cutting measure for emergency care is PQRS #317: Preventive care and screening: screening for high blood pressure and follow-up documented.
PQRS-CAHPS Required for Groups of 100 or More
- CMS has finalized that all groups of 100 or more eligible providers that register to participate in the group practice reporting option, regardless of reporting mechanism the group practice chooses, must also select a CMS-certified vendor to administer the PQRS–Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey on their behalf (formerly known as Clinician Groups–CAHPS).
- This requirement is in addition to all the other group practice reporting options such as “qualified registry.” However, this requirement does not apply to the “qualified clinical data registry” (QCDR) option.
- CMS confirms that, beginning in 2015, it will no longer be feasible for CMS to bear the cost of group practices of 100 or more eligible professionals to report the CAHPS for PQRS survey measures.
2015 PQRS Measure Updates
CMS has retired 50 measures from the PQRS program in 2015, including the following four out of the seven measures from the 2014 emergency care cluster:
- #28: Aspirin for acute myocardial infarction
- #55: 12-lead ECG for syncope
- #56: Community-acquired pneumonia (CAP): vital signs
- #59: CAP: empiric antibiotic
PQRS measures potentially relevant to emergency physicians in 2015 are listed in Table 2. Please review the detailed coding of each measure in the 2015 PQRS Measures Specifications Manual.
Measure-Applicability Validation (MAV) Process
- Eligible providers can still satisfy PQRS and avoid the penalty by reporting on fewer than nine measures but would be subject to the MAV process to determine whether they reported on as many measures as are applicable to the eligible professionals’ practices. The MAV process will also allow CMS to determine whether group practices should have reported on any of the cross-cutting measures.
- Although the measures listed in Table 2 represent nine measures across four domains, not all eligible professionals will see patients for each measure. A performance score of zero will not count toward the nine-measure goal. Therefore, most eligible professionals in the ED will be subject to the MAV process for 2015.
- At press time, CMS had yet to release details for the 2015 MAV process or update the MAV clusters to reflect the changes in the 2015 PQRS measure set but expected to publish the 2015 MAV to the CMS website by mid-January 2015.
Pages: 1 2 | Single Page





No Responses to “Medicare Final Rule Changes 2015 PQRS Requirements”