9. Blow some O’s up the nose, ie, NO DESAT. In most patients (except those with significant shunting and high positive end-expiratory pressure requirements), you will dramatically prolong safe apnea, allowing intubation efforts through the mouth without desaturation.
10. All bets are off in the “surgically inevitable airway.” In situations when ventilation and passive oxygenation are not possible (eg, distorted anatomy, perilaryngeal pathology, and massive fluids from below that preclude supraglottic airways), sometimes the best airway remains a scalpel to the neck.
[/fullbar]
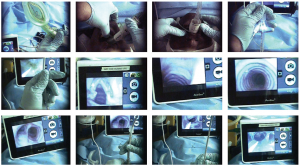
Endoscopy Sequence
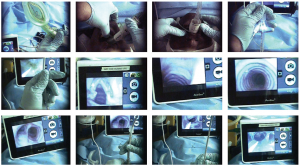
(click for larger image)
Top row (left to right): 1) Loading the tube into the Aura LMA-type airway, placing tip of the tube at the base of bowl; 2) Inserting the Aura into the patient; 3) Seating the Aura by lifting the mandible and using thumbs to push the device in; and 4) Holding the proximal end of tube in place with the third, fourth, and fifth digits, and inserting the AMBU A-scope (endoscope) into the tube using thumb and index finger.
Middle row (left to right): 5) Feeding the scope down the tube; 6) Vocal cords; 7) Passing through cords and looking at the cricothyroid membrane from the inside, with tracheal rings visible below; and 8) Moving down the trachea. Note that the tracheal rings are horseshoe shaped, with membranous trachea (flat) at the bottom.
Bottom row (left to right): 9) Carina; 10) While an assistant holds the endoscope up, the operator rotates it counterclockwise and advances the tube down the scope through the Aura; 11) Full advancement of tube down the Aura, with the distal tip of the tube extending beyond the endoscope; and; 12) View of the distal tube, including the Murphy eye, and the carina as the endoscope is removed. Through the endoscope, the operator can verify tube tip location above the carina and below the cords on endoscope removal.
References
- Warters RD, Szabo TA, Spinale FG, DeSantis SM, Reves JG. The effect of neuromuscular blockade on mask ventilation. Anaesthesa. 2011;66:163-167.
- Calder I, Yentis SM. Could ‘safe practice’ be compromising safe practice? Should anaesthetists have to demonstrate that face mask ventilation is possible before giving a neuromuscular blocker? Anaesthesia. 2008;63:113-5.
- Calder I, Yentis S, Patel A. Muscle relaxants and airway management. Anesthesiology. 2009;111:216-7.
- Kheterpal S, Martin L, Shanks AM, Tremper KK. Prediction and outcomes of impossible mask ventilation: a review of 50,000 anesthetics. Anesthesiology. 2009;110:891-7.
- Parmet JL, Colonna-Romano P, Horrow JC, Miller F, Gonzales J, Rosenberg H. The laryngeal mask airway reliably provides rescue ventilation in cases of unanticipated difficult tracheal intubation along with difficult mask ventilation. Anesth Analg. 1998;87:661-5.
Topics: Airway ManagementCritical CareEmergency MedicineEmergency PhysicianPatient SafetyProcedures and SkillsRapid Sequence Airway
About the Author

Richard M. Levitan, MD, FACEP, is an adjunct professor of emergency medicine at Dartmouth’s Geisel School of Medicine in Hanover, N.H., and a visiting professor of emergency medicine at the University of Maryland in Baltimore. He works clinically at a critical care access hospital in rural New Hampshire and teaches cadaveric and fiber-optic airway courses.
View this author's posts »





No Responses to “10 Tips for Safety in Airway Management”