4. There is no single symptom or sign or combination of clinical features that has adequate predictive value in ruling out testicular torsion.11
Of particular importance is that the presence of a cremasteric reflex does not rule out the diagnosis. Studies report varying sensitivities as low as 60 percent and odds ratios (ORs) from 4.8 to 27.8.12,13 While the presence of an elevated testicle (OR=58.8) and a horizontal testicular lie increase the likelihood of testicular torsion, it is often difficult to palpate the testicle only, thereby determining its position relative to other adjacent structures.14 Scrotal erythema, edema, and testicular swelling are commonly reported in patients with torsion. However, these findings are also commonly found in patients with epididymitis and torsion of the appendix testis.13 Prehn’s sign is the relief of pain with elevation of the testicle, historically thought to be common in patients with epididymitis. This physical examination finding does not reliably distinguish epididymitis from torsion. One cross-sectional study of 120 patients found the Prehn’s sign was present in 91 percent of patients with torsion and 21 percent of those with epididymitis.15
Explore This Issue
ACEP Now: Vol 39 – No 10 – October 2020In 2013, an attempt at combining clinical features of testicular torsion in a clinical decision tool for the diagnosis of testicular torsion yielded the TWIST (Testicular Workup for Ischemia and Suspected Torsion) score. While this score showed a 100 percent positive predictive value when all clinical findings were present, potentially obviating the need for Doppler ultrasound imaging confirmation of the diagnosis, it failed to show adequate negative predictive value in ruling out the diagnosis clinically.16 Hence, all patients with any suspicion for testicular torsion should have urgent Doppler ultrasound imaging and/or urological consultation.
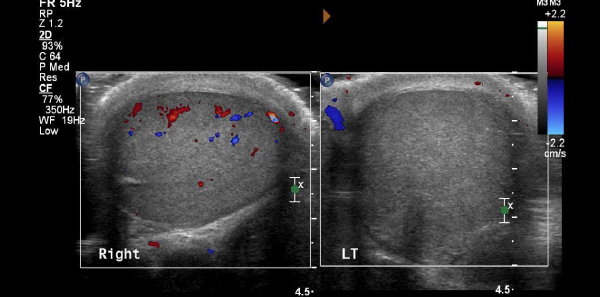
5. Doppler ultrasound has significant limitations in the diagnosis of testicular torsion.
If clinical features cannot rule out torsion, can a Doppler ultrasound? Typically, Doppler ultrasound findings for testicular torsion include an enlarged, hyperemic testicle; decreased Doppler flow to the parenchyma of the testicle itself; and a “whirlpool sign” (a spiral-like pattern of the spermatic cord twisting).17,18 Unfortunately, the test characteristics of Doppler ultrasound are far from perfect, and it is subject to false negatives; the spermatic cord may untwist while the ultrasound is being performed and re-twist afterwards. Alternatively, a partially-torsed testicle may exhibit arterial flow but no venous flow, or it may show an abnormal high-resistance pattern of arterial flow. The sensitivity of Doppler ultrasound ranges from 88 to 100 percent.17 When ultrasound is nondiagnostic and the clinical presentation remains concerning, urology consultation remains warranted. The gold standard for diagnosis and exclusion of testicular torsion is surgical exploration.
Pages: 1 2 3 4 | Single Page



No Responses to “5 Tips on Testicular Torsion”