Explore This Issue
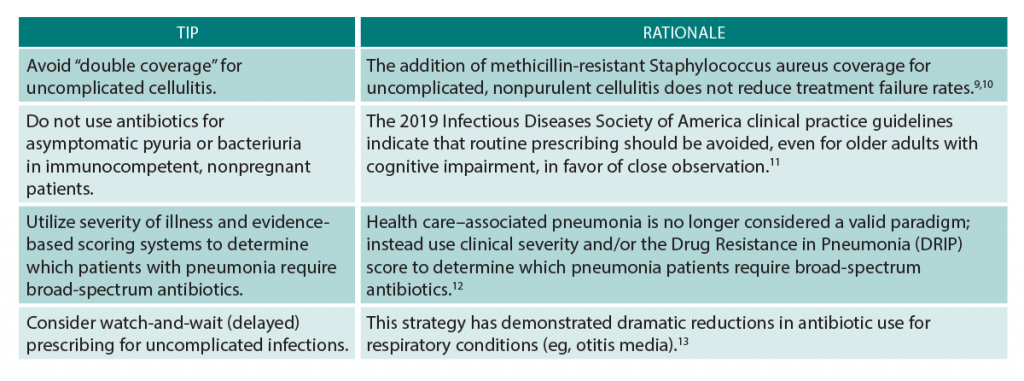
ACEP Now: Vol 39 – No 02 – February 2020(click for larger image) Table 1: Top 5 Tips to Improve Antibiotic Stewardship in the Emergency Department
Become a Champion for Your ED
Ready for the next level? What about becoming an ED antibiotic stewardship champion or starting an ED-specific antibiotic stewardship program? Yes, this is in our wheelhouse!
Hospital antibiotic stewardship programs are now required by The Joint Commission and the Centers for Medicare & Medicaid Services (CMS), and emergency medicine needs to have a seat at the germ-infested table. Practicing at the intersection of the community and the hospital, we are the frontline providers for patients with MDROs. Our role is to try to select the correct initial antibiotic, despite diagnostic uncertainty. This unique and often challenging task requires an informed plan. We, as emergency physicians, should be the ones making the plan, not just following orders from others who don’t have experience doing what we actually do.
For an in-depth implementation guide to antibiotic stewardship in the emergency department, check out the MITIGATE toolkit. This tool takes the Centers for Disease Control and Prevention’s recommended core elements for outpatient antibiotic stewardship (which include a commitment to using antibiotics appropriately, implementing one policy or practice, tracking and reporting, education, and expertise) and adapts them to emergency department and urgent care settings. The toolkit leverages improvement science and behavioral economics to nudge clinicians to do the right thing in avoiding antibiotics for viral infections.
ED champions are critical to any program’s success. Interventions are more effective when they take the unique ED environment and workflow into account.
Still on the fence about leading the antibiotic stewardship charge? There are plenty of other ways you can start to engage beyond day-to-day patient care.
First, make sure someone from your emergency department sits on the antibiotic stewardship committee. Think about how local guidelines and clinical pathways can support better antibiotic use. For instance, do you really need a urine sample in the nurse-driven order set for chest pain? How about working with pharmacy and therapeutics to develop an empiric antibiotic prescribing guide based on antibiograms for your emergency department? The same goes for sepsis order sets, which should include evidence-based empiric antibiotic prescribing decision support. We can even facilitate de-escalation by making sure relevant cultures are ordered.
The goal of antibiotic stewardship programs is to improve patient outcomes, but they can also make your life easier. Find out the pain points to optimizing antibiotic use in your emergency department and then design a simple quality improvement project to fix them. There are a number of stewardship targets to explore, and some of these efforts can be made seamless through the use of behavioral nudging—for example, setting a default duration for antibiotics in your electronic health record by indication or making the first-line agents pop up for the default diagnosis. These fixes are better for patient care, they preserve physician autonomy, and they require fewer clicks. Win-win-win.
The fight against superbugs and MDROs is not coming to our emergency department’s doorstep; it is already here. As the frontline physicians for any epidemic, we will be the ones wearing the hazmat suits, placing the central line to hang the fourth antibiotic, and watching our patients suffer. ACEP has a team of emergency physicians working to prepare antibiotic stewardship resources for our workforce. In the meantime, we ask, Are you ready to step up and be an antibiotic steward? Is your emergency department ready for an antibiotic stewardship program? And before we just throw broad-spectrum agents into an IV, what the heck is the source of that 102°F fever in the patient in bed four?
Pages: 1 2 3 4 | Single Page





No Responses to “5 Tips to Improve Antibiotic Stewardship in Your Emergency Department”