After a three-year saga of flawed public policy, difficult politics, and dangerous regulations, Washington Chapter ACEP is proud to report the success of the “ER is for Emergencies” program, which has achieved unprecedented results. It started in 2010 with a legislative mandate borne out of the necessity to save money in the state budget as a result of the recession. The Washington State Health Care Authority (HCA) proposed a $36 million annual savings through a policy to “just not pay” after the third ED visit judged to be nonemergent in 12 months. Calling ED providers “poor stewards of the health care dollar” in print and making a direct threat to prudent layperson protection, the HCA then went on to create a nonemergent list of 700-plus diagnoses, which included chest pain, hemorrhage with miscarriage, and sudden loss of vision. Despite our attempts to work with the regulators, litigation became the only option to stop the dangerous proposal.
Explore This Issue
ACEP Now: Vol 33 – No 07 – July 2014Washington Chapter ACEP stepped up by engaging more than 90 percent of our providers to create the Washington State Emergency Medicine Action Fund and file suit. National ACEP and the Emergency Medicine Action Fund provided financial support for litigation and experienced researchers to provide data on the dangers. We brought allies including the Washington State Medical Association, Washington State Hospital Association, other physician specialties, and patient advocacy groups. The providers won the battle in court but were committed to helping the state improve care and save money.
A Solution Where Everyone Wins
This was the turning point. While the HCA pushed back, the legislature sought solutions and asked for our ideas. We established ground rules of preserving access to emergency care; protecting the prudent layperson standard; and delivering high-quality, cost-effective care. We realized we first had to invest some money in infrastructure and then build a system around communication. Through advocacy in the capital and the governor’s mansion, an aggressive public relations effort, and tenacity, the legislature passed Bill 2127, creating the Washington State Seven Best Practices:
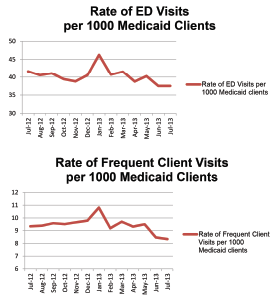
Emergency Department Utilization: Update on Assumed Savings from Best Practices Implementation, March 20, 2014
1. Tracking of ED visits, with an automated notification sent to providers of any patient visiting five or more times in the last 12 months. All hospitals have adopted the program. This tracking includes a summary of prior visits, care plans from any facility in the state, and safety warnings such as violence or radiation alerts.
Pages: 1 2 3 | Single Page





No Responses to “7 Best Practices to Reduce Emergency Department Misuse”