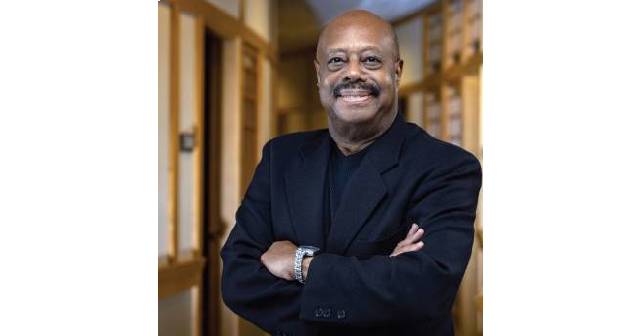
I recently spoke with Ramon W. Johnson, MD, MBA, who is currently the president of the American Board of Emergency Medicine (ABEM). He joined me for our annual conversation between ACEP Now and ABEM to answer some questions from practicing emergency physicians. Our conversation has been edited for space and clarity.
Explore This Issue
ACEP Now: Vol 43 – No 03 – March 2024Dr. Dark: Our profession is composed of over 44,000 ABEM certified emergency physicians, about 96 percent of whom are EM residency trained. I’ve been listening to some of the more senior docs out there, and especially across specialties, many of whom are getting tired of certifying boards and maintenance of certification. They are asking the question, “Why don’t I just get board certified by an alternate board?” Or, in some circumstances saying, “Why don’t I just go ahead and let my certification lapse?” What is ABEM’s value proposition for physicians considering those options?
Dr. Johnson: I truly believe that there is not really an excellent alternative board out there. You may be aware that one of the alternative boards was recently discussed at the AMA and the AMA basically said that [other] certifying board didn’t meet up to the expectations or the quality that they feel is necessary for a certifying board. I think it’s important to understand that certifying boards have a responsibility to the public and it not only means that they must assure initial certification meets a certain standard and that standard needs to be an objective standard, but that continuing certification is also critical for that standard to be met. And very few alternate boards out there are doing anything like that now.
Dr. Dark: Let’s talk a little bit about that initial certification. Conversations among younger physicians have noted that the oral examination is moving from a virtual platform back to an in-person platform. During the pandemic many things transition to virtual, including the oral boards. Why the change back? Why not stay virtual?
Dr. Johnson: It was never the intent that we would continue to have a virtual examination. I do think that if you look at the American Board of Medical Specialties, more than half of the boards do have a type of oral exam and the majority of those that went virtual because of the pandemic have now basically gone back to and in-person exam. When you look at the format of the virtual exam, there’s clearly some limitations in what we can do with that type of format. And we know that we can create a better way of evaluating physicians by going back to in-person. There are some things we just cannot examine adequately in the virtual setting. It’s really, to the benefit, not only of the public but to the physicians, that we go back to an in-person exam.
Dr. Dark: Could you expand a little bit on that, things that you can’t examine in a virtual setting? But also, why oral boards as opposed to just the written certifying exam. What are you actually looking for in order to board certify someone that you get from an in-person oral boards situation?
Dr. Johnson: One of the things we’ve noticed is that there are some additional competencies that are important to emergency medicine and our patients such as patient-centered communications, high stakes and difficult conversations, managing conflict, team management, how you prioritize patients that need to be seen. And probably one of the more important areas that we’re really wanting to investigate more and evaluate better is in procedural skills. These are things we just can’t do in the virtual format. But we now have ways that we can actually evaluate these things once we go back to in-person. As we go back to the new exam that we’re creating, it will not be like the current oral exam. There will be some significant changes.
Dr. Dark: In our February issue, we talked about virtual reality in emergency training –people putting on their little goggles, even 3D printing things like laryngoscope blades, or other devices so that they can actually train in those tactile elements and the procedural elements that defines our specialty. Do you think the oral exam will get replaced by something like that? Do you see that happening in the future?
Dr. Johnson: It’s interesting. We actually convened a summit looking at the future of the oral exam. And at that summit the idea of having some type of virtual reality did come up and there’s certainly an interest in that among some of the stakeholders that participated at the summit. I have gone to some procedural assessment centers where they are actually using virtual reality in some of their simulation exercises and it’s certainly something that is cutting edge. It is something I think is potentially a tremendous benefit as we look at ways that we can evaluate that competency in the future. I’m not sure the technology is quite there yet on the scale that we would like it to be, but it’s something we want to continue to investigate and maybe someday in the future we will see that being utilized.
Dr. Dark: I was looking through the ABEM annual report for 2022/2023, and I saw where it said 700 clinically active physicians volunteered their services to ABEM in that year, usually serving as examiners. Being an academic myself, a lot of people are like, “Why all this free labor?” And I also saw ABEM, their revenue went up $7 million. So why are we relying on volunteers as opposed to compensating people that are donating their time to the Board in order to certify the next generation of emergency physicians?
Dr. Johnson: We do have over 700 volunteers. It would be almost impossible to, if we were paying those physicians to do the work that they do provide for us as volunteers. One of the great honors in being even certified is serving as a volunteer. I started my career as a volunteer doing the oral board exam probably over 30 years ago. And it’s been a tremendous experience just getting together socially with what used to be twice a year in Chicago to have camaraderie with my fellow emergency physicians. And I found that during that time it was amazing the things that you could exchange with your colleagues that ultimately would even make you a better physician.
It is the case that having paid individuals is expensive. We do try and compensate our volunteers by providing airfare, hotel room, and a meal stipend. We do what we can to offset some of that expense, but to pay someone full time I think would be probably an impossibility. Recently, we spent about $10 million putting in a new IT system and technology and this will be something that will provide a greater experience for all of our diplomates. And we continue to invest in various ways to improve providing the services that we provide to all of our diplomates.
Dr. Dark: How are the test takers, the candidates, doing in terms of either their initial certification or their recertifications on things like the ConCert exam that was transitioned to the MyEMCert exam? What topics are of concern to ABEM as it pertains to what we as emergency physicians are not doing well on?
Dr. Johnson: That’s a great question. I would probably have to do some research to see if there are any particular subject areas that are problematic. One of the things that we have tried to do with the continuing certification exam or MyEMCert is to really look at ways that we can expedite knowledge translation into reality. And I think we’ve been extremely happy with the fact that we’ve really tremendously reduced how long it takes for us to take knowledge that’s in the literature and bring it to our practices. In addition to the standard MyEMCert content are key advance questions. The key advances which are really cutting edge things that are happening in the field of emergency medicine, which we can bring immediately to the attention of our diplomates.
We launched several modules this year looking at substance use. These modules don’t qualify for the required modules that are needed to maintain certification but do provide additional education and are tremendously cutting edge. I recently spoke to a diplomate who took one of the modules and he was able to apply it almost instantly in his practice when taking care of patients who came in with drug related problems. We launched a resuscitation module, knowing full well that if there’s one thing that emergency physicians should be doing well, it’s being able to manage resuscitation. And these types of activities, mean you don’t have to be taking an ATLS or an ACLS or a PALS course every so often. It will lead to providing better care to our patients.
Dr. Dark: I have one last question for you and purely asking for a friend here. Do I still have to do the LLSA?
Dr. Johnson: It really just depends upon when your certification expires. We do know that the LLSA is phasing out depending upon when you have to recertify and then we are switching everything over to the MyEMCert modules. It’s always a question when we’re at the Scientific Assembly at the ABEM booth. Many of our diplomates will come by and want to know exactly where they are in the recertification process.
Dr. Dark: Is there anything else that I left out that you wanted to tell ACEP members?
Dr. Johnson: We know that there was a lot of concern about the new certifying exam. I want to let you know that I believe that the next exam we do put into play will be something that will take what your everyday type of practice and translate it exactly into what we’re testing. We want it to be valid, we want it to be reliable. We do think it will really examine those competencies that we currently cannot do only with the written exam or even with our current oral exam. It won‘t launch until 2026, but we’re hoping by that time we’ll be ready to go. We‘ll be using a test center that‘s located in Raleigh, North Carolina. We chose that center because The Board of Anesthesia has been using that center for their own certification needs and they’ve been quite successful, being able to get their diplomates and candidates through the process.




No Responses to “A Conversation with ABEM President Dr. Ramon W. Johnson”