Explore This Issue
ACEP Now: Vol 36 – No 04 – April 2017ILLUSTRATION: Chris Whissen PHOTOS: shutterstock.com
Emergency department providers across the nation recognize that, every shift, patients seem older. These observations are not an illusion. Aging baby boomers will increase the number of older ED patients every year for the next few decades. Vulnerable older patients often arrive to the emergency department with multiple comorbidities and vague chief complaints that require more complex decision making and prolonged evaluation times and increase the likelihood of admissions. ED providers are concurrently pressured to increase throughput and discharge many of these patients.1 Adding the difficulty of navigating the often-complex social issues that come with caring for elder patients, the challenges increase even further. ACEP’s Geriatric Emergency Medicine Section (GEMS) developed geriatric emergency department (GED) guidelines intended to provide recommendations and guidance for optimal geriatric emergency patient care.2 These were endorsed by the ACEP Board of Directors in 2013 and also by several other national emergency medicine and geriatrics organizations.
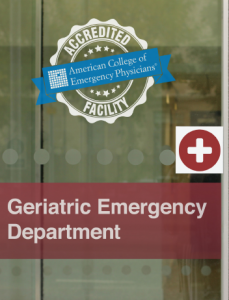
Not all emergency departments are the same, yet optimizing geriatric emergency care across emergency departments of varying sizes and capabilities depends on prioritizing the best practices included in the ACEP GED guidelines. Best elder care depends on aligning GED practices with the resource capacity of one’s hospital and staff as well as the specific needs of one’s patients. In addition, ED leaders can use these recommendations to leverage hospital resources and the support required to care for an aging population safely and efficiently. Increasingly, hospitals are advertising “senior-friendly emergency departments,” but the process of transforming guidelines into actual health care delivery has not been standardized.3 In the fall of 2016, ACEP convened a taskforce (see Table 1) to develop a GED accreditation proposal intended to help members and hospitals provide higher-quality geriatric emergency care under increasingly challenging conditions. This proposal was approved by the Board of Directors in January 2017. Accreditation will be awarded on a three-tier platform as determined by each hospital’s level of implementation of the GED guidelines.
The ACEP GED Accreditation (GEDA) program is intended to be a transparent and minimally disruptive mechanism that assesses and publicly recognizes a hospital’s commitment to optimal geriatric emergency health care delivery. The emphasis here is on hospital responsibility because effective geriatric care requires effective interdisciplinary patient care. Success depends upon giving the emergency department needed support and hospital resources to ensure more comprehensive geriatric evaluations and timely access to follow-up care. Once a hospital commits to support credentialing an emergency department as geriatric-centered, the expectation is that the hospital will also provide and sustain the resources to effect those changes.
Pages: 1 2 3 | Single Page





No Responses to “ACEP Accredits Geriatric Emergency Care for Emergency Departments”