
More than 60 resolutions were put forth during the ACEP22 Council Meeting in San Francisco, with many of them drawing considerable discussion and debate. As usual, the resolutions provided a snapshot of what’s happening in society—concerns about access to reproductive health care, the dangers of scope creep, and appropriate involvement between law enforcement and intoxicated patients, to name a few.
Explore This Issue
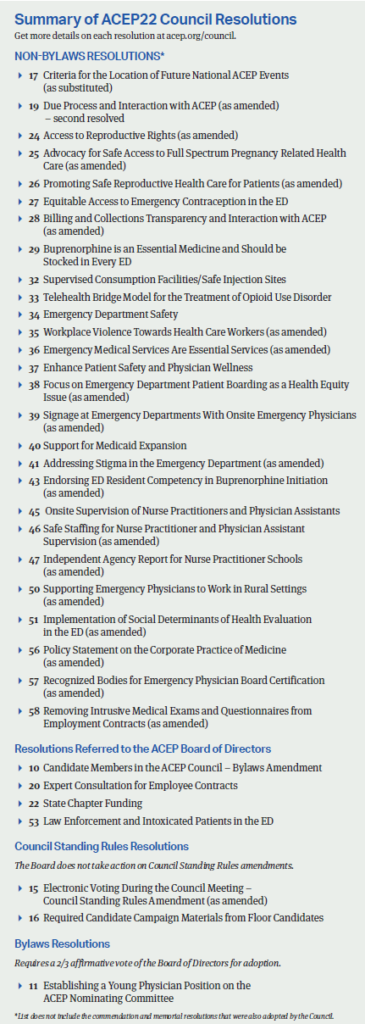
ACEP Now: Vol 42 – No 01 – January 2023A few of the most-discussed topics are highlighted below. View the sidebar to see a list of resolutions approved by the Council or referred to the ACEP Board of Directors. Interested in the work that happens after a resolution is approved? Visit acep.org/council to view actions taken on recent resolutions.
Access to Reproductive Health Care
After the Supreme Court overturned Roe v. Wade in late June 2022, it was no surprise that four resolutions were put forth to the ACEP Council focused on pregnancy-related health care. Taken as a whole, the reproductive health care resolutions called on ACEP to protect both physicians and patients. For patients, that included supporting equitable, nationwide access to evidence-based pregnancy care, including advocating for universal access to emergency contraception. For physicians, the resolutions pushed for clear legal protections for emergency physicians providing federally-mandated emergency care, clinical practices and policies that protect the integrity of the physician-patient relationship, and increased education around pregnancy-related complications.
Despite the potential divisiveness of this topic, the ACEP Council came to a clear consensus: All four resolutions were eventually adopted by the Council. (Resolution 27 was adopted as submitted, while Resolutions 24, 25, and 26 were adopted after amendments.)
Monica Saxena, MD, JD, a clinical assistant professor in the department of emergency medicine at the Stanford School of Medicine, led the writing for “Resolution 26: Promoting Safe Reproductive Health Care for Patients” with a group of her Stanford colleagues who, surprised by the sudden overturn of Roe v. Wade and its implications for emergency medicine, decided to take action through ACEP’s democratic process.
Dr. Saxena and her Stanford colleagues practice in the first hospital in the country to offer abortions through the emergency department (ED), so they are uniquely familiar with the procedure and its protocols. Still, they wanted to think beyond California to write a resolution to address the concerns encountered by colleagues in more restrictive states.
“We understand that emergency physicians are not a monolithic group,” Dr. Saxena said. “We wanted to make sure that we were respecting different opinions and even to some level different state laws and different institutional regulations, while also advocating for our patients.”
Resolution 26 underwent significant amendments during the Reference Committee hearing, with much of the debate around whether to include special emphasis on EMTALA. When it came time for Resolution 26 to be debated on the Council floor, testimony was mostly supportive.
Dr. Saxena said she was braced for strong opposition from some councillors, but the live testimony—even from those who disagreed with the resolution—was constructive and collegial. “That was wonderful to see that people were coming together to advocate for patients,” said Dr. Saxena.
As a newcomer to the ACEP Council process—it was Dr. Saxena’s first time writing a resolution and attending the meeting—she described her experience as eye-opening, educational, and encouraging. “This was just a group of four or five physicians who came together and said, ‘We want to do something, and we pooled our resources and we wrote a resolution, and we got it passed. That’s democracy at its best.”
Scope of Practice
Another hot topic at the 2022 ACEP Council meeting was scope of practice. Four resolutions were debated that covered competencies, offsite supervision, safe staffing and educational standards. Many of the scope of practice discussions had a common theme: How can we ensure ACEP is emphasizing the importance of emergency physician-led care teams without opening the door to unintended consequences?
“Resolution 44: Competencies of Independent Emergency Medicine Nurse Practitioners and Physician Assistants” called for ACEP to adopt policy positions stating that nurse practitioners and physician assistants should never practice emergency medicine without in-person physician supervision. Prior to the meeting, asynchronous testimony overwhelmingly agreed that nurse practitioners (NPs) and physicians assistants (PAs) should not practice without onsite supervision available for support, but comments questioned the practicality of requiring every patient to be seen by an emergency physician in all settings. Heavy debate ensued: How would this policy play out in rural EDs? Could this resolution incidentally create a path for physicians who do not meet ACEP’s definition of an emergency physician? In the end, this resolution was not adopted by the Council.
The Council did reach consensus on the gold standard for supervision when it approved “Resolution 45: Onsite Supervision of Nurse Practitioners and Physician Assistants,” which calls for ACEP to revise its existing policy statement so that onsite emergency medicine physician supervision is stated as the gold standard.
The next scope of practice debate centered on staffing ratios: Should ACEP take the lead, or is this complex, circumstantial issue best left to local medical directors? After lively debate on both sides of the issue, the Council adopted an amended version of “Resolution 46: Safe Staffing for Nurse Practitioner and Physician Assistant Supervision” that called for ACEP to investigate and make recommendations regarding appropriate and safe staffing models of emergency physician-led teams.
ACEP’s EM Workforce Section submitted a resolution to address concerns about the wide variation and quality in nurse practitioner education. “Resolution 47: Independent Agency Report for Nurse Practitioner Schools” called for ACEP to “work with the American Medical Association to provide recommendations for nurse practitioner education reform to improve the quality and standards of nurse practitioner training for the purpose of improving physician-led patient care.” Asynchronous and live testimony was mixed, with commenters discussing alternative approaches such as a minimum number of clinical hours and/or standardized testing. After much discussion, an amended resolution was adopted.
Resolution author and EM Workforce Section leader Deborah Fletcher, MD, FACEP, said hearing from the many perspectives of ACEP Councillors is a learning opportunity. “There are so many serving in the Council who have been doing this longer than I have, and I appreciate the advice. I might get carried away at times and look for immediate results (the ED physician in me!), but it is great to have those who understand the process and how to work for the best outcome long term,” she said.
Law Enforcement and Intoxicated ED Patients
The past few years of ACEP Council meetings have seen resolutions related to the relationship between law enforcement and the emergency department or EMS, and this year was no different. Elizabeth Barrall Werley, MD, FACEP, and Jennifer Savino, DO, FACEP, helped lead a team from the Pennsylvania College of Emergency Physicians that submitted “Resolution 53: Law Enforcement and Intoxicated Patients in the Emergency Department” to help combat workplace violence in the emergency department (ED). Resolution 53 called on ACEP to investigate alternative care models to evaluate patients in police custody, such as telehealth, to determine necessity of an in-person evaluation, and to encourage law enforcement to stay with any patient they choose to bring to the ED who poses a risk to the safety of themself or others until a disposition has been determined or the physician determines assistance is no longer needed.
Dr. Werley was inspired to write the resolution by a scary encounter she had years ago in her ED when she was in her second trimester with her first child. Law enforcement left an intoxicated patient with her because he seemed to be in control. After they left, he physically assaulted her. She ultimately pressed charges and testified in court. “Fast forward 10 years later, and I attended ACEP’s 2022 Leadership & Advocacy Conference where we lobbied for protection from violence against health care workers. So, my personal encounter from over a decade before was fresh in my head all over again [as I proposed this resolution].”
When working on the resolution with fellow PACEP members, Drs. Werley and Savino “noticed a clear dichotomy regarding our experiences with law enforcement among us from those who practice in more urban settings to those that practice in a more small town or rural environment,” said Dr. Werley. Those perspectives prepared them for the detailed debate that ensued at the Council Meeting.
There was concern that the second part of the resolution—that ACEP encourage law enforcement to stay with any patient they choose to bring to the ED who poses a risk to the safety of themself or others until a disposition has been determined or the physician determines assistance is no longer needed—did not reflect the collaborative relationship needed with law enforcement. Those testifying acknowledged that this is a complex problem that affects emergency physicians and patients, and highlighted the practical, regulatory, and legal challenges associated with implementing this resolution. There was additional debate about hospitals taking more responsibility for the safety of staff and patients.
The telemedicine aspect of the resolution “brought up concerns that it could turn into a slippery slope, and we may be asked to do other evaluations for law enforcement,” said Dr. Savino, so it was agreed to remove that part.
The resolution prompted a lot of discussion about the institution’s role in keeping its employees safe, which illuminated the safety resources available to large, urban EDs compared to smaller hospitals.
“I was surprised that some perceived [our resolution] as anti-law enforcement, which was never the intent. I have had great experiences with law enforcement in my career,” Dr. Werley said. “But just like hospitals have various resources based on size and location, the same can be said for a small town with only one or two officers on duty versus a city with a much larger police force.”
After much debate, this resolution was referred to ACEP’s Board of Directors. “We knew it might be contentious when we wrote it, but felt it was worth discussing because it impacts so many of us,” said Dr. Werley. “I’m glad it generated so much discussion because it demonstrated to the Board the importance of this issue.” Both Drs. Savino and Werley were comfortable with the resolution’s outcome, saying they felt confident that the Board had heard both sides of the discussion and would be able to explore the additional nuances of the issue.
Safe Injection Sites
ACEP Past President Larry Bedard, MD, FACEP, believes substance abuse disorder patients should be treated with all available resources and dignity. It’s that belief, combined with his knowledge about California’s safe injection site pilot sites, that led him to co-author “Resolution 32: Supervised Consumption Facilities/Safe Injection Sites” with Dan Morhaim, DO, FACEP.
This resolution called on ACEP to support the development of Supervised Consumption Facilities/Supervised Injection Sites (SCF/SIS) in the United States that would collect data to inform policymakers on the feasibility, effectiveness, and legal aspects of whether these sites in reduce harm and health care costs related to injection drug use.
For this topic, there was an interesting divide between the asynchronous testimony before the Council meeting (unanimously opposed) and the live testimony in San Francisco, which was mostly supportive. The debate centered around whether safe injection sites are a proven method of harm reduction. Some members providing testimony believed ACEP should focus on establishing sobering centers instead.
“I like taking on controversial issues,” Dr. Bedard said. He absorbed the Council’s debate over whether ACEP should support safe injection sites or sobering centers, but he feels it doesn’t need to be framed as an either/or situation. Dr. Bedard thinks they work well together. “There’s a significant number of patients who go to a safe injection center that get referred to treatment centers.”
After the Council adopted the resolution, Dr. Bedard reflected on his long history with the Council—he’s been involved for 40 years—and how important the Council is for setting policy that affects EM physicians and patients. He encourages other ACEP members to get involved. “This is how we set policy,” he said. “It’s where we represent not only the best interests of our fellow physicians, but also of our patients.”
From veteran Council member Dr. Bedard to relative newcomers Drs. Fletcher, Saxena, Savino and Werley, they agreed that participating in the 2022 ACEP Council Meeting was energizing.
“I am glad for the diversity in opinions, but also that we really have patients at the heart of the debate,” said Dr. Fletcher. “[Council] is a truly fascinating process… So much is at stake right now.”
“Before I got involved at the local level, I didn’t even know Council existed. I imagine not a lot of ACEP members even know about it or what is done at the meeting,” said Dr. Savino. Now that she’s participated, she better understands how the debate and discussion helps align the College’s work to find solutions to pressing issues. “At the end of the Council meetings, I feel like I actually made a difference.”
Jordan Grantham is senior content manager at ACEP.




No Responses to “ACEP Council Debates Scope of Practice, Access to Care, Safe Injection Sites, and More”