Times of crisis test the mettle of our leaders and demonstrate the importance of having smart, decisive, compassionate leadership backed by knowledgeable, dedicated advisers and staff.
Explore This Issue
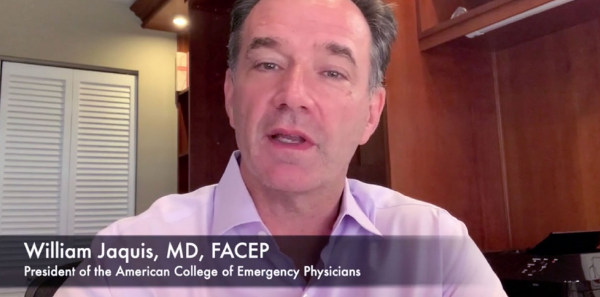
ACEP Now: Vol 39 – No 05 – May 2020When William Jaquis, MD, FACEP, stepped into his role as ACEP President at ACEP19 in Denver, no one could have predicted that SARS-CoV-2, the novel coronavirus that causes COVID-19, would soon be testing him, ACEP, and the whole specialty of emergency medicine.
Dr. Jaquis recently had a call with ACEP Now Medical Editor in Chief Jeremy Samuel Faust, MD, MS, MA, FACEP, to discuss ACEP’s efforts to meet the unprecedented challenge posed by COVID-19. Here are some highlights from their conversation.
JF: How was your term as ACEP president going before coronavirus? What were you focused on before it took over?
WJ: It’s a little hard to remember when there wasn’t coronavirus at this point.
The President takes his presidency at the ACEP annual meeting and from there goes to the Board retreat. There’s a lot of planning at the Board retreat, and some of the committee structure and objectives get worked out as well as task forces.
For the retreat itself, my approach was to be very strategic. We talked about how this is different from being absolutely excellent at something. That probably prepared us for what was to come—not knowing it was to come—because certainly it’s time to be strategic.
Also, there were the three task forces. The first was the future of emergency medicine, where we had a Star Chamber group work through the parameters for that work. It is still going on, although some of it will be deferred.
The second is rural health. As emergency medicine, we have a very big question to answer: For ACEP, are we driven by members and their needs, or are we driven by the whole spectrum of emergency care? We have to walk through what that means when we make choices and have discussions. Rural health is clearly an area where we need more work, so we set up a task force to look at how we can do a better job. Fortunately, there are many people who can help us with this.
The final one is on EM group ownership and private equity.
Those are the things I’m working on.
JF: Turning to the question on everyone’s mind: coronavirus. When did you start to understand that the coronavirus outbreak was going to be more than your average crisis? How did you respond when you had that realization?
WJ: I don’t know that I’ll mention a date. There are key points in time for me. The first was when it hit our shores and how hard it hit our shores. It was clear we weren’t ready. When it hit Washington state is when we knew it was here. We had no way to change the course of it at that point—it was going to be pretty widespread. We just had to see the severity of it.
The other piece is, as young people started to get sicker, the question of who is safe from this virus and why. We still don’t know that answer. Those were the key points where it was pretty clear it was going to be widespread and there was going to be a big question of how we might restratify people and how we might take care of ourselves, frankly.
JF: Knowing that hindsight is 20/20, is there anything that we could have done differently in January or February?
WJ: The problem in emergency medicine is we start to see things and it’s a little while before people prove them. With places like the CDC [Centers for Disease Control and Prevention], the cases that they objectively say are COVID, that they define as COVID, so many people attach to that information and it’s hard to get them out of that thinking. But there are two things, and they are not any secret. The first is more widespread testing to see what it is we had, and where, and who. That’s still an issue.
The other piece is, once we started to recognize the severity of disease and how widespread and difficult it was, the production and distribution of PPE [personal protective equipment], and that’s still a problem as well. Now it’s clear how disrupted the production supply chain has been. The fight we’re all having with each other to get that type of equipment should be better coordinated.
Even in emergency medicine, we may have taken a while to figure out that this is not “just another flu.” And even though 85, 90 percent of the people are going to have mild disease, we don’t know which 85 or 90 percent that is.
JF: How is ACEP making a difference in this moment? How do you balance the need to maybe criticize leadership in government when they’re not responding quickly enough with the need to keep that communication line open?
WJ: I’m not big on criticism honestly. In the hot wash afterwards, or the debriefing, we can be critical. The question now is how we get things done. I don’t know that it’s necessary for me, at least in this position, to be critical but more to be a voice for what we need and how we need to get it and where we need to get it and to stay open to whatever avenue we can to do that.
We do a ton of work both out front and behind the scenes with many federal agencies, CDC, HHS [Department of Health and Human Services], CMS [Centers for Medicare & Medicaid Services], even The Joint Commission, the FDA [Food and Drug Administration], the White House, and all of our elected leadership both on the state and federal levels. In order to have that continued dialogue and to keep that white hat messaging for us, we have to stay a little bit out of the criticism. Quietly, we can be critical, but we really are looking, with everything we do, to say: How can we get this? Where’s the supply chain? How can we help? How can we use our chapters? Our staff is working on this seven days a week, 12 hours a day, if not more, trying to figure out all those pieces of behind-the-scenes work we have to do in order to get things done.
JF: Can you give our members a sense of some wins that we’ve had recently?
WJ: Certainly telemedicine is a win. That separates us from people who are infected. It allows some of our sites to decompress, potentially, from things that don’t have to come to their department and do so in a way that recognizes how we have to do it and where we have to do it. It removes some of those EMTALA constraints and also allows us to effectively bill for it.
The other piece where I’m optimistic is the issue of payments. One thing that’s pretty concerning is the drop in volume in a lot of places. How do we make up for some of that drop in volume? We’ve been working hard on that with multiple entities to look at other payment methodologies. It’s not a win yet, but we’re getting a good audience. Every industry is looking at how they can stay solvent, stay afloat. We are doing the same thing for our physicians, which I think is going to be huge.
JF: Once we get through this crisis, what do you think the major take-home messages will be for emergency physicians and medicine in general? Is this an opportunity for our field to enhance our presence in the national conversation about health care both now and in the future?
WJ: I think it can be, but a lot of that has to do with how we react. We have this period of time where people are looking at us in a very, very favorable way for the work that we do. It’s work we know we do all the time, but it’s more evident when there’s this huge crisis. But riding that wave means some additional work that we can’t forget. That has a lot to do with how we look at our expertise but also our ability to advocate. As physicians, take this anxiety and anger you feel now, which is so justifiable, and channel it into something that leads you to continued action after we finish.
One of the things we’re starting to set up already is how we can inform whoever is going to make those decisions about what it is we really need. We, as emergency medicine, need to be in that discussion on how we prepare for what might be next and have people understand what we do and its value. We need people to continue (if they are already doing it) or start (if they’re not) going beyond the clinical piece by telling our stories, by getting involved with advocacy. All of those pieces will really help us in the future.
JF: On a personal level, are you getting any sleep? Are you able to do the things that you enjoy doing, the things you love outside of medicine, or is that on hold and it’s COVID-19 all the time?
WJ: I think it’s on hold for a lot of us. Am I getting some sleep? Gov. Cuomo said it fairly well. How are you going to sleep when we’re in the middle of these crises? We have people that need the work we do, and so I do get some sleep, but it’s not what I will get when this is all done. And the things I love—again, I don’t think any of us are able to do them right now.
On the other hand, one of the things that is happening is reestablishing what things are important to us and understanding how, on a day-to-day basis, we might take them for granted and figuring a way, at the end of this, to reestablish those components. We are at the tip of the spear and at the front lines in this, but there are a lot of people working in support of us as well—from those people working grocery stores to the people working in our apartments with us. And so it’s important to understand how grateful we are to them as well and be able to express that gratitude.






No Responses to “ACEP President Dr. Jaquis Discusses Meeting the COVID-19 Challenge”