
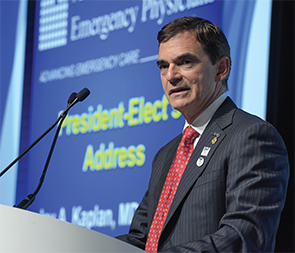
Each year brings new challenges for our specialty to face and a new President to lead the charge. Jay A. Kaplan, MD, FACEP, who took over as ACEP President in October, recently shared his views on a few of those challenges with ACEP Now Medical Editor-in-Chief Kevin Klauer, DO, EJD, FACEP. Here are some excerpts from their conversation.
Explore This Issue
ACEP Now: Vol 35 – No 03 – March 2016KK: What do you think the biggest challenges facing emergency physicians are?
JK: I think the biggest challenge for emergency physicians, and for ACEP as well, includes continuing to show our value both to our patients and to those who pay for the care, the federal government and insurers. We continue to be labeled as the most expensive place to receive care. It is very clear that the major driver of health reform is not really quality—it’s cost. I find it very interesting that what used to be called the Patient Protection and Affordable Care Act, passed in 2010, is now being called the Affordable Care Act. The greatest challenge is to give great care to our patients with the limited resources that we have. We are going to continue to be asked to do more with less.
KK: Congratulations on Emergency Medicine Wellness Week. What additional goals do you have for your presidency?
JK: Emergency physicians lead all specialties in terms of burnout. Burnout can be characterized as a loss of work fulfillment, emotional exhaustion, and a sense of disconnection or depersonalization. We have to continue to focus on that and helping physicians be more healthy. Wellness isn’t a one-week thing; it’s a yearlong thing.
Fair reimbursement. There was a bill in Congress and there are bills in multiple states that talk about “surprise billing.” Insurance companies have been fairly effective in portraying physicians as greedy doctors, predatory billers, and that we are sending bills to patients over and above what the insurance company is willing to pay. Unfortunately, the concept of fair payment doesn’t play well with regulators and legislatures because they think that doctors are already well paid. I think that we have to stop talking about surprise billing. We have to start talking about surprise coverage. As one insurance VP said at one of the American Medical Association meetings I recently attended, “The first and only thing which patients look at is the affordability of the premium.” Insurance companies have hoodwinked patients by offering them “affordable premiums” but raising their deductibles. One of my top goals is to go after the insurance companies and portray them as more interested in profits than they are in patients.
 There are a number of other areas we are also very focused on to provide better care for patients. One is the opioid crisis, where more patients are dying from prescription drug overdoses than they are from motor vehicle accidents. In the age of terrorism, ACEP needs to take leadership, so I formed a high-threat, high-casualty task force that will look at what ACEP can do to be leaders in educating the public and physicians on how to deal with active-shooter incidents.
There are a number of other areas we are also very focused on to provide better care for patients. One is the opioid crisis, where more patients are dying from prescription drug overdoses than they are from motor vehicle accidents. In the age of terrorism, ACEP needs to take leadership, so I formed a high-threat, high-casualty task force that will look at what ACEP can do to be leaders in educating the public and physicians on how to deal with active-shooter incidents.
KK: Occasionally, people have been critical of you when you speak about experience of care so passionately, as you have done a fair amount of consulting work in that area. How would you respond to those criticisms?
JK: I have been a patient advocate for a long time, and as emergency physicians, we do ourselves harm if we try to separate ourselves from that. There is good evidence that the more patients trust us and the better their experience is, the more they are compliant with our recommendations, and they’ll have better outcomes. I have never been one to say that you have to satisfy every patient. I think we need to give patients what we feel is in their best interest, not necessarily what they want. I would also respond that I have never been an advocate for patient satisfaction in the absence of being an advocate for creating a great place for doctors and nurses to work. Unhappy doctors don’t make for happy patients. Whenever I travel to do consulting, those who experience the work find that I am an advocate for them to ensure they receive the adequate resources that they need to give great care to their patients. This year, I have dramatically cut down on consulting work. I’ve wanted to devote time to being President of ACEP. My wife and I planned for that, as my income would be significantly cut, and that’s fine with me.
KK: Let’s talk about ACEP and membership value. How would you explain to a member why ACEP is spending the College’s money on a new headquarters?
JK: Membership value. We recently had a study of our membership and, within the next two months, are creating a plan to improve retention of our transitioning residents through the first 10 years of their practice. ACEP brings educational value with eCME, ACEP CME Tracker, and Portfolio Tracker that allows you to track all of your credentials.
 Our current building is over 30 years old. We have outgrown it, with some staff having offices across the street. The building doesn’t say, “You should have respect for the physicians who practice emergency medicine.” Because we had a couple of good years in terms of ACEP14 and ACEP15 and have been able to save money, it makes all the sense in the world to create a new headquarters with new technology that will have all of our staff under one roof and is a place that says emergency medicine is a special specialty and physicians who practice emergency medicine are to be honored. We will have an area for the history of emergency medicine, and we will have an outside area sponsored by our Emergency Medicine Foundation that will have pavers with messages from emergency physicians.
Our current building is over 30 years old. We have outgrown it, with some staff having offices across the street. The building doesn’t say, “You should have respect for the physicians who practice emergency medicine.” Because we had a couple of good years in terms of ACEP14 and ACEP15 and have been able to save money, it makes all the sense in the world to create a new headquarters with new technology that will have all of our staff under one roof and is a place that says emergency medicine is a special specialty and physicians who practice emergency medicine are to be honored. We will have an area for the history of emergency medicine, and we will have an outside area sponsored by our Emergency Medicine Foundation that will have pavers with messages from emergency physicians.
KK: Will this expense have a negative impact on any programs that members currently benefit from?
JK: Absolutely not. Under the leadership of Dean Wilkerson, Craig Price, Bobby Heard, Michele Byers, and Gordon Wheeler in Washington, and the countless other staff members, there is not a specialty organization that could have a better staff. They’re passionate about emergency medicine and represent us well. The new headquarters will not compromise any of our activities and, in fact, will help us be more efficient in addressing other issues.
KK: What are your thoughts about democracy, and how important do you feel that is in the current emergency medicine climate?
JK: I’ve been part a democratic group for my entire emergency medicine career, with the exception of about two years when I was part of the health system. Democracy does not mean anarchy, that everybody is equal, or that you don’t have leadership. I think the fundamentals of the best of democratic groups relate to physicians having a say in their practice environment and open books providing physicians some sense of where their compensation is coming from. If they work hard and they give their patients great care, they should be compensated more than those who do less. There’s no one model that is best. In this age of consolidation of insurers and physician practices, and more doctors becoming employed, we are going to see those changes in emergency medicine. We need to maintain the sense of physicians as owners rather than renters. In other words, physicians should feel that they have some responsibility for their work environment. Any model that promotes that is a model that we need to support.
I think the biggest challenge for emergency physicians, and for ACEP as well, includes continuing to show our value both to our patients and to those who pay for the care, the federal government and insurers. We continue to be labeled as the most expensive place to receive care. It is very clear that the major driver of health reform is not really quality—it’s cost. —Jay A. Kaplan, MD, FACEP
KK: I have one last question for you, Jay. How do you see the role of the emergency physician changing in the near future and beyond?
JK: What brought us to this dance ain’t going to get us into the next one. Einstein said the best definition of madness is to do things the same way and expect different results. How do most of us approach change? Change is good; you go first. I think we have to go first, and so I think the role of emergency medicine will change. I think that retail clinics will have huge backing from venture capital. I think they and urgent care will continue to take the less-sick patients away. With the incidence of heart disease, diabetes, and obesity, and people living longer, we’re going to have plenty of patients to see. Our practice is going to become more difficult because we’re going to see sicker patients.
As emergency physicians, we need to own telehealth and telemedicine. I think we are the best specialists to provide video and over-the-phone consultation with patients. I think we’re going to be utilizing advanced practice providers more and more because I think we’re going to have to leverage our expertise and leverage our time. It will be incumbent upon us to be careful in regard to our supervision of our advanced practice providers to ensure that our patients continue to get great care while, perhaps, expanding their scope. Health care is a team sport, so I think we’re going to need to learn more about managing complex systems and leading groups of people. I think we have a very bright future. Two F words: I think we need to be fascinated about the challenges that we face and fight for our patients.
Editor’s Note: Read more about Dr. Kaplan’s goals (ACEP login required).
Pages: 1 2 3 4 | Multi-Page




No Responses to “ACEP President Dr. Jay Kaplan Discusses Challenges Facing Emergency Medicine”