In February 2018, the ACEP Board of Directors approved a revised clinical policy on the evaluation and management of adult patients presenting with suspected acute venous thromboembolic disease.1 The policy is available at www.acep.org/patient-care/clinical-policies.
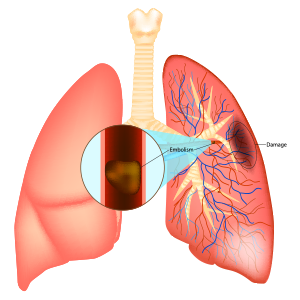
Venous thromboembolism (VTE), including both deep venous thrombosis (DVT) and pulmonary embolism (PE), is a major public health problem. Undiagnosed, untreated patients are believed to be at substantial risk for progressive disease and sudden death typically because of worsening right-sided heart strain and ultimately cardiovascular collapse. Treated patients are at risk for chronic sequelae (ie, vein scarring, leg swelling, and pulmonary hypertension) and adverse events from ongoing anticoagulation (ie, hemorrhage and other medication adverse effects).
One significant challenge for health care providers evaluating patients for VTE lies in the variability of signs and symptoms of the disease that are related to clot burden, location, and the individual patient’s cardiopulmonary reserve. Without perfect, cost-effective tests for the diagnosis of VTE, providers have come to rely on Bayesian decision making to guide their workup, using pretest probability to interpret diagnostic evaluations and generate posttest probability of disease. Doing this allows providers to maximize diagnostic accuracy while minimizing over-testing and patient harm from the risks associated with unnecessary evaluation and treatment.

Table 1. Translation of Classes of Evidence to Recommendation Levels
Efforts to refine this Bayesian approach in emergency medicine have been ongoing. Original studies to determine pretest probability and the accuracy of various screening tests have been validated, and the limits of their efficacy are being explored. Additionally, substantial efforts are being made to advance the treatment of VTE by balancing outcomes, anticoagulation risks to patients, and patient preferences. Non–vitamin K antagonist oral anticoagulants (NOACs) are particularly appealing for long-term anticoagulation because of their simple oral dosing regimens with no need for routine laboratory monitoring.
This most recent revision investigates five areas of interest or controversy in the evaluation and management of VTE. The first two critical questions address the role of unique clinical prediction rules and age-adjusted D-dimer testing in the diagnosis of PE, and the remaining three questions focus on optimal treatment and disposition for individuals receiving a diagnosis of venous thromboembolic disease.
For each critical question, a structured literature review was performed, evidence was systematically graded (see Table 1), and evidence-based recommendations are presented.
Critical Questions
Question 1. In adult patients with suspected acute PE, can a clinical prediction rule be used to identify a group of patients at very low risk for the diagnosis of PE for whom no additional diagnostic workup is required?
Pages: 1 2 3 | Single Page




2 Responses to “ACEP Revises Venous Thromboembolism Clinical Policy”
August 4, 2019
Erik Auf der Heide, MD, FACEPThis policy needs to define:
1) all acronyms
2) low, intermediate, and high risk
August 6, 2019
Dawn Antoline-WangPlease visit https://www.acep.org/patient-care/clinical-policies/ to download the full policy.