It also includes the numbers of available inpatient hospital beds, psychiatric beds, and designated pediatric specialty centers because greater capacity in those areas can alleviate crowding and boarding within emergency departments. Because one of the most commonly cited concerns in emergency departments across the country is the lack of access to on-call specialists, this category also includes measures of the total supply of commonly requested specialists, including neurosurgeons; orthopedists; hand surgeons; plastic surgeons; and ear, nose, and throat specialists.
Explore This Issue
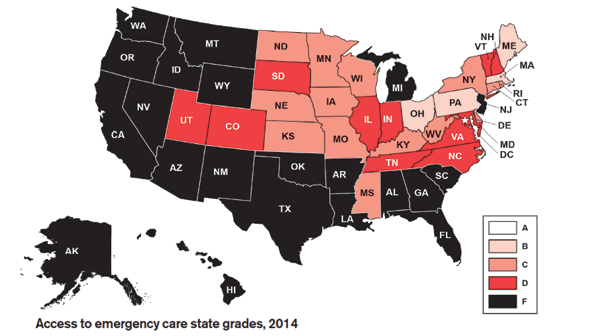
ACEP Now: Vol 33 – No 02 – February 2014“America’s grade for Access to Emergency Care was a near-failing D- because of declines in nearly every measure,” said Jon Mark Hirshon, MD, MPH, PhD, FACEP, the chair of the task force that directed development of the Report Card. “It reflects that hospitals are not getting the necessary support in order to provide effective and efficient emergency care. There were 19 more hospital closures in 2011, and psychiatric-care beds and hospital-inpatients beds have fallen significantly, despite increasing demand. People are increasingly reliant on emergency care, and primary care physicians are advising their patients to go to the emergency department after hours to receive complex diagnostic workups and to facilitate admissions for acutely ill patients.”
The Report Card includes several national recommendations, including requests to:
- Fund the Workforce Commission, as called for by the Affordable Care Act (ACA), to investigate shortages of physicians, nurses, and other health care professionals.
- Pass the Health Care Safety Net Enhancement Act of 2013, H.R. 36, introduced by Rep. Charlie Dent (R-Pa) and the companion legislation, S. 961, introduced by Sen. Roy Blunt (R-Mo). This legislation would provide limited-liability protections to (emergency and on-call) physicians who perform the services mandated by the federal EMTALA law, which requires emergency patients be screened, diagnosed, and treated regardless of their insurance status or ability to pay.
- Fund pilot programs, provided for in the ACA, to design, implement, and evaluate innovative models of regionalized, comprehensive, and accountable emergency care and trauma systems.
- Support and fund the mission of the Emergency Care Coordination Center at Department of Health and Human Services to create an emergency-care system that is patient and community-centered, integrated into the broader health-care system, high quality, and prepared to respond in times of public health emergencies.
- Withhold federal funds to states that do not support key safety legislation, such as motorcycle helmet laws and .08 blood alcohol content laws.
- Fund graduate medical education programs that support emergency care, especially those related to addressing physician shortages in disadvantaged and rural areas.
- Support efforts to fund emergency care research by the new Office of Emergency Care Research under the National Institutes of Health.
- Hold a hearing to examine whether additional strains are occurring in the emergency department safety net as a consequence of the ACA.
For a full list of recommendations, to see state grades, and to see how you can help, go to www.emreportcard.org.
Pages: 1 2 3 | Single Page





No Responses to “ACEP’s 2014 Report Card on Emergency Medicine Reveals Major Access-to-Care Deficit”