Explore This Issue
ACEP Now: Vol 34 – No 02 – February 2015(click for larger image)
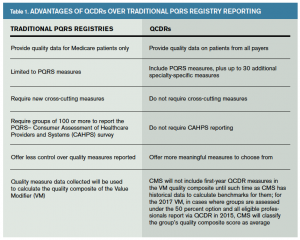
Table 1. Advantages of QCDRs Over Traditional PQRS Registry Reporting
What Are the Benefits of Participating in a QCDR?
ACEP submitted an application to meet CMS requirements for PQRS and QCDR reporting by the Jan. 31, 2015, deadline for the PQRS 2015 performance year/reporting period. Use of the registry under PQRS and QCDR will minimize or avoid negative financial reimbursement from CMS.
With the transition to a value-based system upon us, in which health service providers are paid based on quality of care, efficiency, patient satisfaction, and outcomes, the QCDR will provide a means for providers to track such parameters from patient encounter information they already document, then adjust practice as necessary to maintain compliance with the highest of standards. PQRS was introduced by CMS to evaluate patient outcomes and quality of care. PQRS registries, and now QCDRs introduced in 2014, are considered key vehicles to automate the reporting of data to qualify for full Medicare Fee-For-Service reimbursement. Private payers are also moving to collect these quality measures to evaluate agreements with providers.
With participation from emergency clinicians nationwide, data from the QCDR will be used to generate regular feedback reports that summarize local practice patterns and treatment outcomes as well as compare an ED’s patterns with those of a number of others across the nation. The reports could also be used to identify process-of-care variables that may correlate with key patient outcomes.
Stacie Schilling Jones is director of quality and health information technology in the public affairs division of ACEP in Washington, D.C.
Pages: 1 2 | Single Page




One Response to “ACEP’s Qualified Clinical Data Registry Helps Physicians Meet PQRS Goals”
August 7, 2015
AMA, CMS Announce ICD-10 Grace Period Specifics - ACEP Now[…] so long as codes from within the right family are used, nor will CMS penalize physicians under the Physician Quality Reporting System for the […]