A clinical data registry records information about the health status of patients and the health care they receive in an organized system. Clinical data registries collect uniform data (administrative, clinical, patient-reported, and other data) to evaluate specified clinical processes and outcomes. Clinical data registries typically focus on patients who share a common reason for needing health care. Registries have emerged as valuable solutions for harnessing the power of information technology to capture statistically relevant, evidence-based data to aid in decisions regarding the most optimal patient care. Information from registries may also be used to compare the performance of health care providers with regard to their patient outcomes.
Explore This Issue
ACEP Now: Vol 34 – No 02 – February 2015What Is a CMS Qualified Clinical Data Registry?
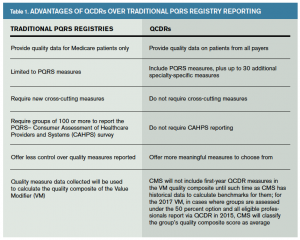
The 2012 American Taxpayer Relief Act authorized a new standard for individual eligible professionals to satisfy Physician Quality Reporting System (PQRS) reporting requirements beginning in 2014. This new mechanism recognizes satisfactory participation in a qualified clinical data registry (QCDR) in lieu of reporting traditional PQRS measures to the Centers for Medicare & Medicaid Services (CMS). QCDRs may submit information on both PQRS measures and up to 30 additional non-PQRS specialty-specific measures. Also, QCDRs give a better picture of the overall quality of care provided because they collect and report quality information on patients from all payers, not just Medicare patients.
For 2015, CMS has retired four of the five PQRS measures most commonly reported by emergency physicians. Simultaneously, it continues to up the ante by requiring nine measures across three domains, with up to 6 percent of Medicare reimbursements at risk for most emergency physicians.
Why Is ACEP Providing a Clinical Data Registry?
ACEP’s mission is to promote the highest quality of emergency care. For 2015, CMS has retired four of the five PQRS measures most commonly reported by emergency physicians. Simultaneously, it continues to up the ante by requiring nine measures across three domains, with up to 6 percent of Medicare reimbursements at risk for most emergency physicians. The timing is right for emergency physicians to be among the early adopters in strategically deploying information technology to drive quality-improvement objectives. Table 1 outlines the advantages of QCDRs over traditional PQRS registry reporting.
Can ACEP Deliver a Quality Information Technology Solution?
ACEP is partnering in the development of a clinical data registry with FIGMD, Inc., a company that specializes in integrating practice management, billing, and coding software as well as electronic health records (EHRs) with registries. FIGMD has developed and maintained registries for the American College of Cardiology, the American Academy of Ophthalmology, and the American Urological Association; has completed integration projects for more than 50 major EHRs; and is capable of working quickly with new practice management, billing, coding, and EHR systems.
Building a Bridge to the Future for PQRS Reporting
The ACEP QCDR is being designed to build a bridge for emergency physicians from the claims-based reporting of the past to the electronic clinical quality measures (eCQMs) of the future. During the 2015 pilot of ACEP’s Clinical Data Registry, we will continue to focus on collecting quality data codes from claims and administrative data sets and begin testing e-measures for future reporting periods. By building this bridge, we anticipate that most participants should be ready to report a mix of administrative and electronic clinical quality measures to CMS for the 2016 reporting period. ACEP’s goal is to have all emergency clinicians reporting eCQMs by the 2017 reporting period, which is when CMS intends to completely eliminate the claims-based reporting mechanism. As ACEP develops more eCQMs for emergency care and more EDs are integrated with the registry, the administrative burden on coders and billers to submit quality data codes should be significantly alleviated.
What Are the Benefits of Participating in a QCDR?
ACEP submitted an application to meet CMS requirements for PQRS and QCDR reporting by the Jan. 31, 2015, deadline for the PQRS 2015 performance year/reporting period. Use of the registry under PQRS and QCDR will minimize or avoid negative financial reimbursement from CMS.
With the transition to a value-based system upon us, in which health service providers are paid based on quality of care, efficiency, patient satisfaction, and outcomes, the QCDR will provide a means for providers to track such parameters from patient encounter information they already document, then adjust practice as necessary to maintain compliance with the highest of standards. PQRS was introduced by CMS to evaluate patient outcomes and quality of care. PQRS registries, and now QCDRs introduced in 2014, are considered key vehicles to automate the reporting of data to qualify for full Medicare Fee-For-Service reimbursement. Private payers are also moving to collect these quality measures to evaluate agreements with providers.
With participation from emergency clinicians nationwide, data from the QCDR will be used to generate regular feedback reports that summarize local practice patterns and treatment outcomes as well as compare an ED’s patterns with those of a number of others across the nation. The reports could also be used to identify process-of-care variables that may correlate with key patient outcomes.
Stacie Schilling Jones is director of quality and health information technology in the public affairs division of ACEP in Washington, D.C.
Pages: 1 2 | Multi-Page




One Response to “ACEP’s Qualified Clinical Data Registry Helps Physicians Meet PQRS Goals”
August 7, 2015
AMA, CMS Announce ICD-10 Grace Period Specifics - ACEP Now[…] so long as codes from within the right family are used, nor will CMS penalize physicians under the Physician Quality Reporting System for the […]