On inspection of the guideline-based diagnostic criteria of pericarditis listed below, one can plainly realize that each of the criteria can occur in patients with other more deadly diagnoses.3 For example, pleuritic chest pain is common in pulmonary embolism. As explained above, pericardial friction rub can be misinterpreted as present in hirsute patients. New widespread ST elevation can occur in MI. New or worsening pericardial effusion can occur with aortic dissection.
Explore This Issue
ACEP Now: Vol 41 – No 07 – July 2022The diagnosis of pericarditis requires two out of four of the following criteria:3
- Pericarditis chest pain—typically sharp, pleuritic, positional
(greater than 80–90 percent of cases)
- Pericardial rub on auscultation (less than one third of cases)
- New widespread ST elevation or PR depression on ECG (up to 60 percent of cases)
- New or worsening pericardial effusion (up to 60 percent of cases)
Additional supporting findings:
- Elevation of markers of inflammation (e.g., C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), white blood cell (WBC) count)
- Evidence of pericardial inflammation by imaging technique (contrast computed tomography, cardiac magnetic resonance)
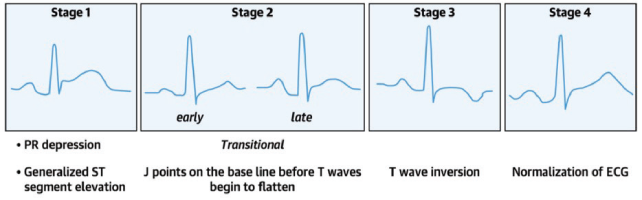
The ECG findings of pericarditis, in particular, may be confused with early repolarization and acute MI. It is important to understand that the ECG findings in patients with pericarditis evolve through four stages (see image) and that patients may present during any of the stages.4 The classic diffuse ST elevation/PR depression (Stage 1) is found in only 60 percent of patients. The evolution of the four changes over time is highly variable and some patients may skip directly from Stage 1 to Stage 4 (normalization). In addition, uremic pericarditis typically does not cause significant inflammation of the epicardium, hence the ECG and the inflammatory markers are more likely to be normal in this subgroup of patients.
Here is a list of ECG features that may help to distinguish pericarditis from MI and early repolarization.5–8 Nonetheless, all of these findings can be seen in patients with cardiac ischemia, underlining again the importance of approaching pericarditis as a diagnosis of exclusion.
- Widespread/diffuse PR depression and/or ST elevation (STE)
- J-point in pericarditis is usually sharper compared to a more blurred J point in MI
- STEs are more commonly convex shaped in ST-elevation myocardial infarction (STEMI), while concave upwards ST elevations are more typical of pericarditis
- If STE or PR depression is present, there is typically a preservation of the normal upright T-waves in pericarditis (note however, that Stage 3 is defined by T-wave inversions)
- STE is rarely >5mm in pericarditis
- ST depressions in V1 and aVR favor pericarditis
- aVL ST segment is typically elevated in pericarditis while aVL ST depression is highly specific for inferior MI
- STE II>STE III favors pericarditis while STE III>STE II is highly suspicious for inferior STEMI
- Spodick’s sign (80 percent of patients with acute pericarditis and five percent of MI) is characterized by down-sloping from the T wave to the QRS segments with the terminal PR segment depressed; this is best seen in lead II and the lateral precordial leads.
Distinguishing ECG findings of pericarditis versus early repolarization:
Pages: 1 2 3 4 5 | Single Page




No Responses to “Acute Pericarditis: A Diagnosis of Exclusion”