- PR deviation strongly favors pericarditis
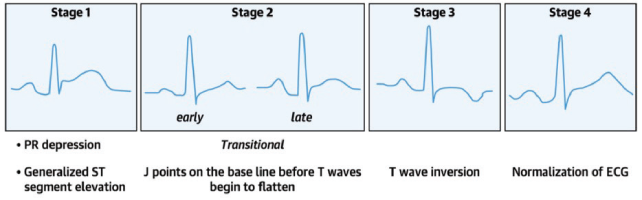
- Evolution of ST and T changes strongly favors pericarditis
- STE: T-wave amplitude ratio >0.25 has a 100 percent positive predictive value and negative predictive value for pericarditis
- Pericarditis STE is typically more evenly distributed and sometimes more prominent in the inferior leads, whereas early repolarization STE is more prominent in anterior leads.
Troponin, in one study, was elevated in one third of cases of pericarditis, and is often associated with STE on ECG and pericardial effusion.9 Inflammatory markers (WBC, ESR, and CRP) are elevated in up to 80 percent of cases, but these markers are not sensitive or specific for the diagnosis of acute pericarditis.10 Patients with elevated CRP are at higher risk for recurrence and should be treated in a timely and aggressive manner.11
Explore This Issue
ACEP Now: Vol 41 – No 07 – July 2022Prevention of recurrence is perhaps the most important aspect of ED treatment of acute uncomplicated pericarditis because recurrence leads to long-term morbidity. Colchicine is the mainstay of ED treatment of acute pericarditis and has been shown in multiple randomized control trials to decrease recurrence and long-term morbidity.12–15 A common cause of recurrent pericarditis is inadequate treatment of the first episode. Up to 30 percent of patients with idiopathic acute pericarditis who are not treated with colchicine will develop either recurrent or incessant disease. Outpatient management of presumed viral/idiopathic uncomplicated pericarditis should include the following:
- Restrict strenuous physical activity (as exercise may trigger recurrence of symptoms)
- Ibuprofen 600–800 mg three times daily or indomethacin 50 mg three times daily
- Colchicine 0.6 mg daily for <70 kg, twice daily for ≥70 kg
- Proton pump inhibitors for those at high risk of upper gastrointestinal bleeding
Duration of uncomplicated pericarditis treatment is usually one to two weeks and is based on resolution of symptoms and normalization of CRP, typically followed by a taper of medications. Corticosteroids should be considered only as a second-line option after nonsteroidal anti-inflammatory drugs (NSAIDs) in patients with absolute contraindications to or failure of NSAIDS because of the risk of chronicity of disease and drug dependence with steroids.
Next time you are faced with a patient with chest pain in the ED, first, rule out other more deadly causes of chest pain first (understanding that there are no clinical features specific to pericarditis), carefully scrutinize the ECG (realizing that no finding is 100 percent specific for pericarditis), and if you arrive at a diagnosis of uncomplicated viral or idiopathic acute pericarditis, be sure to start the patient on colchicine and NSAIDs and also ensure tight follow-up to monitor the clinical course and consideration of serial CRP measurements.
Pages: 1 2 3 4 5 | Single Page




No Responses to “Acute Pericarditis: A Diagnosis of Exclusion”