Once trust is established and patients are willing to accept calming medication, emergency physicians should consider these guiding principles.
Explore This Issue
ACEP Now: Vol 42 – No 07 – July 2023First, oral administration is preferred, as this route can often be as effective as intramuscular administration.6,7 Oral medications are typically cheaper, easier for the patient, reduce the risk of needlesticks, and limit plastic waste.
Second, to avoid increased side effects, the dosing should usually start lower, especially for elderly patients. Treatment should typically begin with just one agent, rather than multiple different medications.8
Third, patients may express a preference for a specific medication or dose based on prior experience. As long as this request is not for a narcotic or other medication with potential secondary gain, it should be respected if feasible.
Fourth, ED treatment should be approached as the first step in a long-term treatment plan, and not as an isolated decision confined to just the ED stay. This means that for patients who have outpatient prescriptions, preference should be given to reinitiating those medications in the ED if feasible, instead of starting a different regimen.
Finally, other interventions focused on comfort should also be considered. These might include medications such as ibuprofen, acetaminophen, or nicotine patches. Meals should be offered, especially if the patient will have a prolonged stay. Environmental stimuli, such as noise and light, should be minimized as possible.
Exceptions

Click to enlarge.
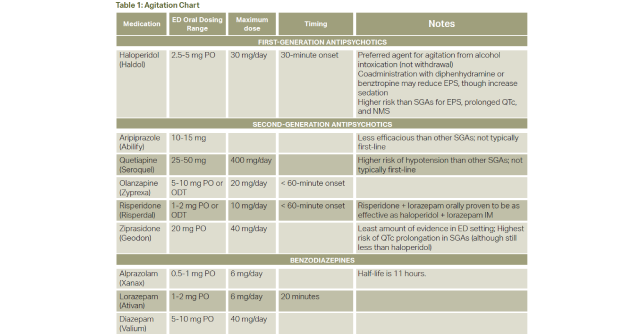
Certainly, each of these guiding principles has clear exceptions, and treatment decisions are at the discretion of the ED physician. For patients with mild to moderate agitation, treatment often begins with second generation antipsychotics (SGAs).9–11 Surprisingly to many ED physicians, these meds are preferred over first-generation antipsychotics (FGAs) such as haloperidol given a lower risk of extrapyramidal symptoms and QTc prolongation. Common injectable SGAs with evidence in the ED setting include olanzapine or ziprasidone, or if oral, risperidone. Of these, olanzapine and ziprasidone are most frequently used in the ED setting for mild to moderate agitation. Aripiprazole for acute agitation is approximately as efficacious as lorazepam, and quetiapine has a higher risk of orthostatic hypotension. Table 1 reviews common dosing regimens and notable side effects.
Benzodiazepines are also frequently used, though ideally not concomitantly with SGAs in patients who have alcohol intoxication.12 Benzodiazepines are ideal for patients whose agitation is due to stimulant use or alcohol withdrawal. They may also be preferred in patients with an unknown etiology for agitation. However, when agitation is due to an underlying psychiatric disorder, SGAs are preferred.
Pages: 1 2 3 4 | Single Page





One Response to “Agitation Treatment in the Emergency Department”
July 12, 2023
John SmithI appreciate the article’s emphasis on the importance of early intervention in the treatment of agitation. Agitation can quickly escalate, so it is important to intervene early to prevent a patient from becoming more aggressive or violent.