“Appendicitis is an obstructed, ischemic ticking time bomb of a finger-like extension of the bowel, which if not urgently removed will burst and lead to death.”
Explore This Issue
ACEP Now: Vol 36 – No 04 – April 2017For more than 100 years, this understanding guided practice and patient expectations, with appendectomy becoming the most common emergency surgery.
We are now learning this was wrong.
New evidence suggests that appendicitis can be cured with antibiotics alone, avoiding surgery. Perhaps hospitalization can be avoided, too, like we manage some cases of acute diverticulitis.
Surgery became available in the late 1800s, and as anesthesia became more effective, appendectomy became routine. When antibiotics were introduced decades later, their use made appendectomy safer. The first clue that antibiotics could cure appendicitis came from experience among young submariners. However, it’s only been in the past few years that researchers have conducted studies in which patients with appendicitis were randomized to receive antibiotics first or urgent appendectomy.
There have been seven European randomized trials, the largest a study from Finland involving 530 participants with results published in JAMA.1 Adults with localized, uncomplicated appendicitis were enrolled. These trials found no increased rate of perforation or sepsis, and there have been no reported deaths in the antibiotics groups. Participants treated with antibiotics returned to their normal activities one to two weeks sooner than those treated with appendectomy. However, about 10 percent initially failed to improve, requiring surgery, as did about another 15 percent who had recurrence over the next year, totaling a 25 percent subsequent appendectomy rate overall. Similar findings have been reported in children from studies in which treatment was not randomized but guided by parent and patient preference.
This year, our group at Olive View-UCLA Medical Center reported our findings on the first US randomized trial in the Annals of Emergency Medicine.2 This study, funded by the National Institutes of Health, was a pilot study of 30 patients with imaging-confirmed, acute, uncomplicated appendicitis. This study’s innovation was the premise that standard postoperative milestones for hospital discharge—clinical stability, oral intake, pain control, and ability to follow up—should be applied to both groups, including the antibiotics group, even when met as early as during the ED stay. We initially gave a dose of long-acting parenteral antibiotic ertapenem to ensure active treatment while the patient’s bowel infection was recovering. Then we had the patients complete a 10-day antibiotics course with oral cefdinir and metronidazole, and we prescribed around-the-clock ibuprofen and prn oxycodone.
We found that of 15 adults randomized to antibiotics, 14 achieved stability in the emergency department and were discharged home. All antibiotics-treated participants had their symptoms of acute appendicitis resolve. Like previous trials, we found antibiotics-treated participants recovered much sooner than those treated surgically. Remarkably, about one-third were pain-free and could return to their normal activities after only one day. Many patients would like to avoid surgery, and of course, eliminating hospitalization would also substantially reduce costs.
Over the next year, two antibiotics-treated participants developed recurrent appendicitis; one had surgery, and the other elected to take another antibiotics course and has remained well. So in this small pilot, our one-year appendectomy rate for antibiotics-treated patients was less than 10 percent.
Is ED management and discharge of acute appendicitis ready for prime time? No. However, emergency physicians should be familiar with antibiotics management since some surgeons are early adopters. Also, the topic of antibiotics treatment of appendicitis has been exposed in the lay press; some patients are now inquiring and even demanding this treatment.3
Before antibiotics treatment is mainstreamed, we need to know much more. Comparing against modern endoscopic appendectomy, it must be clearly established that antibiotics lead to no more complications. We need to better understand how patients value permanently curing the disease compared to minimizing that disease’s impact on their life. We also don’t know how much time to give antibiotics to work. One reason we think we saw no initial antibiotics failures in our pilot study was that, with ED discharge, there was less opportunity for surgeons to observe variation in pain control and offer patients appendectomy. We don’t yet know conclusively in which patients antibiotics are more likely to work.
We are now conducting the first multicenter, randomized US trial called Comparing Outcomes of Drugs and Appendectomy (CODA, ClinicalTrials.gov: NCT02800785). Our methods are similar to our pilot study. This work is being done under a Patient-Centered Outcomes Research Institute grant and in collaboration with the University of Washington Department of Surgery in Seattle.
The results of this study will be important in determining if acute appendicitis should be routinely managed from the emergency department like acute diverticulitis. It appears that we are on the verge of a new type of shared decision making with our ED patients, turning the previous understanding about the most common “surgical emergency” on its head.
 Dr. Talan is professor of medicine in residence (emeritus) at the David Geffen School of Medicine at UCLA, chairman emeritus of the department of emergency medicine, and faculty in the division of infectious diseases at Olive View-UCLA Medical Center in Los Angeles.
Dr. Talan is professor of medicine in residence (emeritus) at the David Geffen School of Medicine at UCLA, chairman emeritus of the department of emergency medicine, and faculty in the division of infectious diseases at Olive View-UCLA Medical Center in Los Angeles.
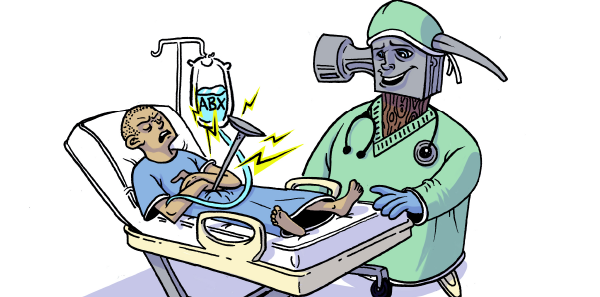
 Adam Talan, the artist who created the article’s illustration, is Dr. Talan’s son. He obtained his degree in Illustration from Academy of Art University in San Francisco and currently works in Los Angeles. You can see more of his work and contact him at adamtalan.com. Adam still has his appendix.
Adam Talan, the artist who created the article’s illustration, is Dr. Talan’s son. He obtained his degree in Illustration from Academy of Art University in San Francisco and currently works in Los Angeles. You can see more of his work and contact him at adamtalan.com. Adam still has his appendix.
References
- Salminen P, Paajanen H, Rautio T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA. 2015;313(23):2340-2348.
- Talan DA, Saltzman DJ, Mower WR, et al. Antibiotics-first versus surgery for appendicitis: a US pilot randomized controlled trial allowing outpatient antibiotic management (published online ahead of print Dec. 11, 2016). Ann Emerg Med.
- Kolata G. Antibiotics resurface as alternative to removing appendix. The New York Times. May 18, 2015.
Pages: 1 2 3 | Multi-Page





2 Responses to “Antibiotics May Be Effective for Managing Appendicitis”
April 30, 2017
Robert Bostic, PA-C, HMC(SS) USN RETGreat article.
The use of iv abx in the treatment of appendicitis, is the mainstay of treatment used by Independent Hospital Corpsmen in Submarine Service since the early 1980’s. Diagnosis was done by physical exam and lab studies, with treatment started on high probability cases. Due to the nature of operations, often sailors were not able to be medivac’d until after symptoms and treatment resolve. We used a 3 drug protocol of ampicillian, cipro, flagyl with excellent results. Most of sailors treated with this protocol, subsequently under went elective appendectomy, due to the nature of submarine operations.
May 7, 2017
Lee Morissette, PA-C, HMCM(SW), USN RetAgreed a great article and the subject of antibiotic use for appendicitis in the United States has been long in coming. As mentioned in the article and posted prior by a reader, fellow PA and former IDC, in the Navy we have long used antibiotics for acute appendicitis treatment, with no significant adverse outcomes. Even if there was a perforation, the patient was stabilized until they could be medevac’d to surgeon. Diagnosis was made on detailed physical exam and a manual CBC as no imaging available on all but larger ships. I personally had several Sailor’s with acute appendicitis that did exceptionally well with the 3 drug regiment previously mentioned.