Minute ventilation is not only relevant to pulmonary function and oxygenation, it can affect acute and chronic acid-base balance. Blowing off CO2 increases pH through the conversion of bicarbonate and hydrogen ions to CO2 and H20 (via the carbonic anhydrase reaction). While most ED patients with high minute ventilation have hypoxemia, some patients with respiratory distress have normal pulse oximetry and clear lungs. Their high minute ventilation is to compensate for an underlying severe metabolic acidosis. Compensatory respiratory alkalosis is common in diabetic ketoacidosis, acute renal failure (from rhabdomyolysis and other causes), and salicylate toxicity.
Explore This Issue
ACEP Now: Vol 34 – No 01– January 2015I now appreciate that 15 Lpm via a non-rebreather mask may not meet the minute ventilation of patients in extremis; this explains how a non-rebreather can collapse with inspiration and why many patients feel suffocated with a mask over their face.
At the other extreme of minute ventilation are patients with chronic obstructive pulmonary disease (COPD) and asthma, who have very low minute ventilation. Their problem is not oxygenation and not acid-base related; it’s primarily a problem with air egress. The inability to get air out prevents getting air in, and hyperinflation (breath stacking) results.
I now make minute ventilation a standard part of my airway assessment. In patients who are placed on noninvasive mechanical ventilation, the machine provides the actual minute ventilation directly. I frequently use noninvasive mechanical ventilation as part of preintubation oxygenation in the sickest of patients, especially if PEEP is required. Very high minute ventilation values should trigger suspicion of an acid-base issue. Significant metabolic acidosis (and a compensatory respiratory alkalosis) is usually identified from chemistry values or a blood gas. In my experience, patients with high minute ventilation from respiratory alkalosis often do not have subjective dyspnea, even though their breathing pattern is evidently abnormal to any observer. This is especially true of salicylate poisoning. Severe salicylate poisoning has impressive hyperpnea (excessively deep breathing) with marked tachypnea.
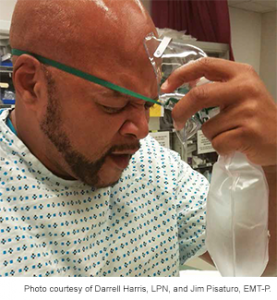
Figure 2.
Think about minute ventilation and oxygenation when patients are intolerant of a non-rebreather. The patients are telling you the flow rate through the mask is not meeting their minute ventilation, and they do not want to re-breathe their CO2. Adding nasal cannula (under the face mask) when treating hypoxemia (and preoxygenating prior to intubation) boosts flow rate, washes out CO2, and significantly increases the effective FiO2.
Normal minute ventilation cannot be used to exclude the presence of severe acidosis, however. Some patients present so fatigued from increased work of breathing when they can no longer compensate; as they tire out and CO2 rises, they become increasingly lethargic. I try to include an elevated CO2 in my differential for lethargy and altered mental status. CO2 retention is easily overlooked, particularly in patients without hypoxia who have baseline mental status problems and limited communication. Hypoxemia is a late manifestation of hypercarbia. Always consider opioid intoxication when patients present with hypoventilation.
Pages: 1 2 3 4 5 | Single Page






One Response to “Avoid Airway Catastrophes on the Extremes of Minute Ventilation”
January 16, 2021
Dr. onkar ThakurVery informative and practical, Thanks to Dr. Richard. Please keep me posted.