Hip fractures are one of the most frequently encountered complaints in the emergency department, with more than 300,000 patients hospitalized annually in the United States.1 Hip fractures significantly increase the short- and long-term morbidity and mortality of older patients.2 Especially in older patients, the pain from this injury is often undertreated, leading to further morbidity, such as increased delirium and delays in recovery.3 Current evidence strongly suggests that multimodal analgesia can decrease morbidity and mortality for patients with hip fractures.4,5
Explore This Issue
ACEP Now: Vol 41 – No 02 – February 2022It has become common practice for emergency physicians to manage the pain from hip fractures with a combination of systemic analgesics and femoral nerve blocks (FNBs) or fascia iliaca blocks (FIBs). These blocks classically target the femoral nerve and have shown moderate analgesia. However, these blocks may provide incomplete pain relief since the articular branches that supply the hip joint originate more proximal to where the FNB/FIBs are performed.
A New Technique for Hip Injuries
The pericapsular nerve group (PENG) block may be a superior regional block for such injuries in the emergency department. This block was originally described in 2018 for total hip arthroplasties, later used for degenerative hip disease, and recently expanded for traumatic hip and pelvic fractures.6 Also, in the emergency department, the PENG block may be the ideal block for pain control for rami fractures. Anatomical research confirms that the PENG block reaches these additional articular branches from the femoral and obturator nerves, which innervate the hip by depositing local anesthetic within the myofascial plane between the psoas muscle and superior pubic ramus.7
The PENG block may be the ideal regional block for such hip injuries in the emergency department as it can be performed rapidly, provides excellent pain relief, and spares motor function deficits often seen with femoral nerve blocks.
Anatomy and Innervation
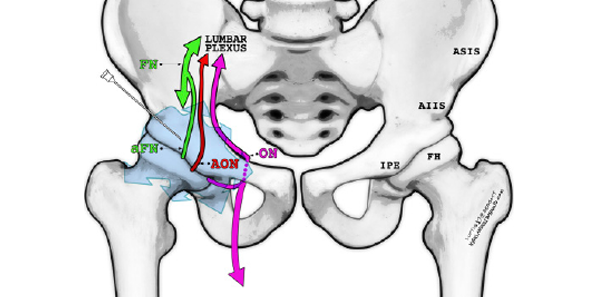
The PENG block targets the terminal sensory branches of the femoral, obturator, and accessory obturator nerves, which are primarily responsible for hip and pelvis innervation. The location of these structures relative to the pelvis is depicted in Figure 1. These nerves branch off proximally from the lumbar plexus and travel deep within the pelvis. Therefore, they are not reliably affected by the more distal FNB/FIB.8
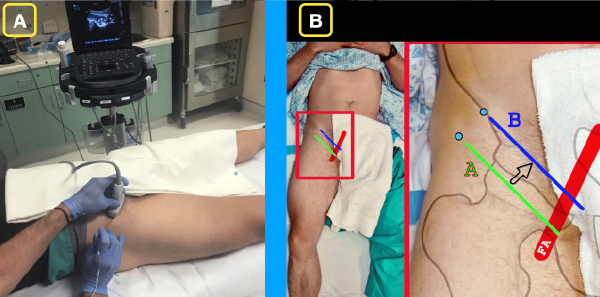
Figure 2A: The ultrasound system is placed contralateral to the affected hip so that the operator has a clear line of sight of the needle as well as the ultrasound screen.
Figure 2B: Basic position of the ultrasound transducer in the region of the inguinal ligament. The green line (A) indicates the first position. In this position, the femoral head and femoral artery will be located. The blue line (B) indicates a minor adjustment in order to locate the ideal location for the PENG block.
Specifically targeting these articular sensory nerves within the myofascial plane of the psoas muscle and ilium can provide superior pain control for hip fractures while also avoiding most of the motor deficits associated with FNB/FIBs. Additionally, anesthetizing the obturator nerve at this level can provide pain control for fractures involving the rest of the pelvis, in particular pelvic rami fractures.9
Supplies
- Low-frequency curvilinear transducer (5-2 MHz) allows for greater visualization of surrounding landmarks. In thin patients and when learning to locate relevant anatomy, we recommend a high-frequency linear transducer (13-6 MHz).
- Anesthetic: approximately 20–30 mL bupivacaine 0.5 percent (5 mg/mL; maximum 2 mg/kg); lower volumes for hip fractures and higher volumes for pelvic fractures. In large-volume plane blocks, always refer to a reputable weight-based local anesthetic (LA) dosing chart such as HighlandUltrasound.com or MDCalc.com.10,11
- Normal saline flushes 10–20 mL. Can be mixed into the same syringe with the LA or injected separately to initially open up the fascial plane (hydrodissection).
- 100-mm 21 g blunt-tip block needle or 20–22 g Quincke spinal needle. Needle visualization for deep target blocks is significantly easier when using echogenic block needles.
- 91-cm or 36-inch tubing.
- Chlorhexidine skin prep.
- Transparent dressing (Tegaderm) for the transducer and sterile gel packets.
- 25–30 g needle for local skin wheal.
Procedure
Pre-block
The patient should be placed on continuous cardiac monitoring and pulse oximetry whenever performing a high-volume ultrasound-guided nerve block. Additionally, the clinician should be knowledgeable of the signs, symptoms, and treatment of local anesthetic systemic toxicity (LAST) and have 20 percent lipid emulsion therapy readily available for this rare but potentially serious complication.12
Positioning
The PENG block is performed with the patient in a supine position. Place the ultrasound system contralateral to the affected hip to allow for clear line of sight. An in-plane lateral to medial approach will allow the operator to visualize the needle tip during the entire procedure (see Figure 2A).
Survey Scan
Place the curvilinear transducer parallel to and over the inguinal crease. Identify the femoral vessels medially and the rounded anterior surface of the femoral head laterally (see Figure 2B). The femoral nerve, which is not targeted in the PENG block, lies just lateral to the femoral artery. While maintaining the same orientation parallel to the inguinal crease, slide the transducer cephalad until the bony ilium is visualized. Also note the anterior inferior iliac spine (AIIS) and iliopubic eminence (IPE) (see Figures 3A and 3B). The rounded hyperechoic psoas tendon (PT) resides along the ilium between these two structures. The target of the PENG block is the fascial plane over the ilium just lateral and deep to the psoas tendon. Note that the femoral vessels and nerve are both medial and far from the needle pathway.
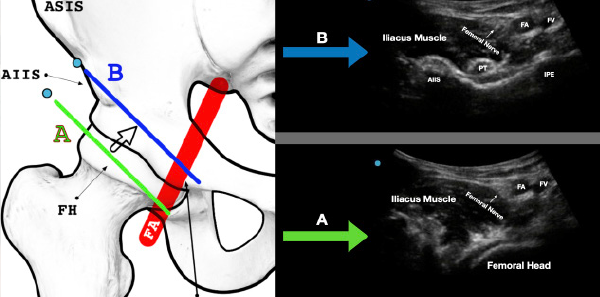
Figure 3A: The green line (A) indicates the initial location. Note the femoral artery (FA) and femoral vein (FV) as well as the femoral head.
Figure 3B: Maintaining the probe parallel to the inguinal crease, slide the probe a bit cephalad. The blue line (B) indicates the ideal location for the PENG block. Note the anterior inferior iliac spine (AIIS), the iliopubic eminence (IPE), and the psoas tendon (PT). The femoral vasculature (FA/FV) and femoral nerve in the proximal aspect of the ultrasound screen will often be visible at this location.
Skin Wheal
After satisfactory identification of the landmarks noted on the survey scan, widely prep the skin with chlorhexidine. Allow this to completely dry and place 2–3 mL lidocaine skin wheal 2–3 cm lateral to the transducer.
Needle Entry
Using a lateral to medial in-plane approach, advance the block needle at a 30 degree to 45 degree angle toward the bony ilium just deep and lateral to the psoas tendon. After the first 1–2 cm, the angle may be slightly redirected to reach this target. With deep blocks that require steep trajectories such as the PENG block, needle visualization may be difficult. “Toeing in” the transducer so that the ultrasound beam is more parallel to the needle can improve visualization.13 Continue advancing the needle until it reaches the hard bony backstop of the ilium. After aspiration, gently hydrodissect this overlaying fascial plane. Proper needle placement will demonstrate anechoic fluid of LA injected underneath the psoas tendon, lifting it upward and spreading medially. If resistance is encountered during injection or fluid is not visualized entering the fascial plane, this can be corrected by slightly rotating the needle and reattempting injection until proper spread is visualized. This needle rotation repositions the needle-tip bevel and assists with penetration into the fascial plane. Once satisfied with the needle placement, slowly inject the remainder of the 20–30 mL of local anesthetic into the already-open fascial plane (see Figures 4 and 5).
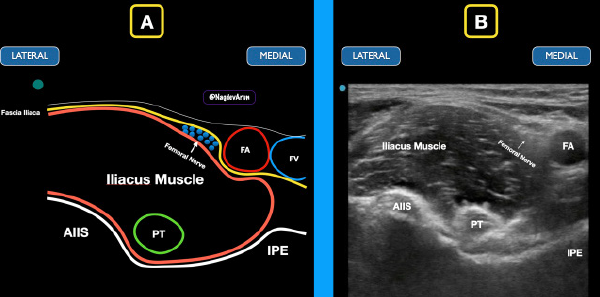
Figure 4: Schematic drawing (A) and ultrasound image (B) of the classic location of the PENG block. Note the fascia iliaca in relation to the femoral nerve, femoral artery (FA), and femoral vein (FV). Note the anterior inferior iliac spine (AIIS), iliopubic eminence (IPE), and psoas tendon (PT).
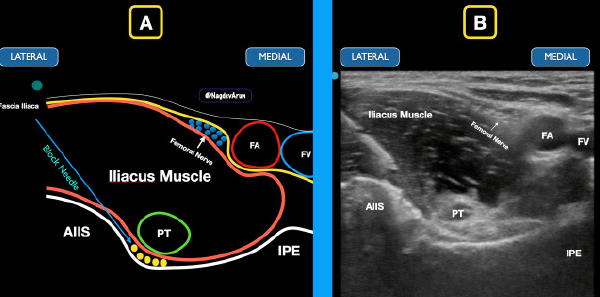
Figure 5: The block needle comes from a lateral to medial approach to deposit anesthetic under the iliacus muscle. The goal is to spread anechoic anesthetic (yellow circles) under the psoas tendon between the iliacus muscle and the bony ramus.
A Simple, Safe, and Valuable Tool
The PENG block is a simple, safe block that can be applied to a wide variety of painful pelvic injuries. It is unique in that this block provides pain control to hip and pelvic fractures and can be a valuable tool for multimodal pain control in the acute setting. This block may provide superior analgesia to hip fractures compared to the traditionally performed FNB/FIBs. Like other ultrasound-guided nerve blocks, the clinician should be knowledgeable about the surrounding anatomy and comfortable with needle visualization.
Dr. Leu and Dr. Sobrero are both ultrasound fellows at Highland Hospital; Josh Luftig, PA, is a clinical instructor at Highland Hospital; Dr. Mantuani is the ultrasound fellowship director at Highland Hospital; and Dr. Nagdev is director of the ultrasound division at Highland Hospital.
References
- Healthcare cost and utilization project (HCUP). Agency for Healthcare Research and Quality website. Accessed Dec. 1, 2021.
- Bentler SE, Liu L, Obrizan M, et al. The aftermath of hip fracture: discharge placement, functional status change, and mortality. Am J Epidemiol. 2009;170(10):1290-1299.
- Titler MG, Herr K, Schilling ML, et al. Acute pain treatment for older adults hospitalized with hip fracture: current nursing practices and perceived barriers. Appl Nurs Res. 2003;16(4):211-227.
- Beaudoin FL, Haran JP, Liebmann O. A comparison of ultrasound-guided three-in-one femoral nerve block versus parenteral opioids alone for analgesia in emergency department patients with hip fractures: a randomized controlled trial. Acad Emer Med. 2013;20(6):584-591.
- Ritcey B, Pageau P, Woo MY, et al. Regional nerve blocks for hip and femoral neck fractures in the emergency department: a systematic review. CJEM. 2015;18(1):37-47.
- Luftig J, Dreyfuss A, Mantuani D, et al. A new frontier in pelvic fracture pain control in the ED: successful use of the pericapsular nerve group (PENG) block. Amer J Emerg Med. 2020;38(12):2761.e5-2761.e9.
- Short AJ, Barnett JJG, Gofeld M, et al. Anatomic study of innervation of the anterior hip capsule: implication for image-guided intervention. Reg Anesth Pain Med. 2018;43(2):186-192.
- Acharya U, Lamsal R. Pericapsular nerve group block: an excellent option for analgesia for positional pain in hip fractures. Case Rep Anesthesiol. 2020;2020:1830136.
- Carr M, Hoffman T, Lin J. Pericapsular nerve group (PENG) block for patients with hip or pelvis fractures in the ED. ACEP Emergency Ultrasound Section website. Accessed Dec. 1, 2021.
- What med? Highland Ultrasound website. Accessed Aug. 13, 2021.
- Local anesthetic dosing calculator. MDCalc website. Accessed Nov. 24. 2021.
- Weinberg G. LipidRescue website. Accessed Nov. 24, 2021.
- Schultz C, Yang E, Jefferson J, et al. Tips for performing ultrasound-guided nerve blocks in the emergency department. ACEP Now. 2021;40(6).





No Responses to “Benefits of Using the Pericapsular Nerve Group (PENG) Block”