Explore This Issue
ACEP Now: Vol 34 – No 05 – May 2015(click for larger image)
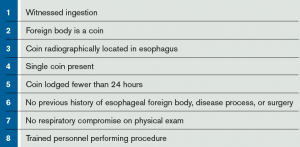
Table 1. Inclusion Criteria for Esophageal Bougienage15,18
Data on the use of glucagon in impacted esophageal coins is relatively sparse. In 2001, Mehta et al prospectively evaluated the use of glucagon and found it to be ineffective in dislodging impacted esophageal coins.13 While the study was double-blind and placebo-controlled, the enrollment of only 14 patients limits its applicability and influence. Emergency physicians, at this point, cannot endoscopically remove a coin, and most of the published literature surrounding Foley catheter removal is done by other specialties (ie, otolaryngology, gastroenterology, surgery). When the right patient is selected, bougienage is a low-risk, highly successful alternative to the previously mentioned interventions and one we can employ in the emergency department.
Bougienage
Bougienage has been around for decades, but it remains an infrequently used modality for the treatment of retained esophageal coins.14 In the correctly selected patient, as detailed in Table 1, bougienage has a success rate of 83–100 percent in advancing the coin into the patient’s stomach.14–18 Among larger studies with more than 100 patients undergoing bougienage, the success rate is 94–95.4 percent.15,19 Rigid adherence to the inclusion criteria maintains bougienage as a reliable modality. However, when not following these criteria, the success rate drops to 75 percent, as Allie et al demonstrated in their 2014 article.15
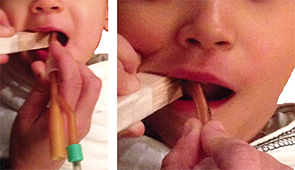
Figure 3. Insertion of the apparatus into the oropharynx.
Written parental consent was obtained for this simulated procedure. Additionally, this demonstrates that if your child is guilty of pocketing a quarter, you could go after it in the comfort of your own home.
Perhaps more important, throughout the previous studies, complications directly related to bougienage are nearly unheard of. Arms et al attempted bougienage on 372 patients, two of whom had the complication of intraoral abrasions from the bite block used during the procedure.19 Additionally, Allie et al demonstrated a minor complication rate of 16.8 percent in their 137 bougienage attempts.15 The majority of these minor complications resulted from vomiting, gagging, or the need for repeat bougienage, without major complications noted. To the best of our knowledge, there has not been a documented serious or life-threatening complication from attempted bougienage.14–19 In addition to the safety and efficacy of bougienage, there have been numerous reports of the decreased cost and length of stay with bougienage versus endoscopy. The length of stay is decreased 4–20 hours and is associated with a decrease in cost of $1,890–$6,000.15–17,19,20 This procedure is not limited to otolaryngology, gastroenterology, or surgery; trained emergency physicians have proven that we, too, can bougienage with the best of them, with success rates of 94–100 percent.14,18,19
Bougienage Procedure
Equipment
- Tape measure
- Tongue depressors (approximately 5–6) taped together to act as a bite block (Figure 1)
- Hurst dilator (Figure 2) or alternative as described here.
- Topical anesthetic (ie, benzocaine spray)
- Water-based lubricant
Procedure
- Confirm that the patient has an esophageal coin with a two-view radiograph and that the patient meets the criteria for bougienage (see Table 1).
- Measure the distance from the patient’s nares to the epigastrium and mark this distance on the Hurst dilator to approximate how far to insert the dilator.
- Topically anesthetize the patient with benzocaine spray.
- Sit the patient upright with a sheet held tightly around the patient and with either an assistant or a parent holding the patient’s head still by the forehead.
- The makeshift bite block constructed earlier can now be inserted to protect the Hurst dilator and allow unobstructed entry of the Hurst dilator into the oropharynx.
- Place a liberal amount of water-based lubricant on the Hurst dilator, or the alternative device, and insert it into the oropharynx (see Figure 3). Advance it until you reach the mark you placed on the dilator. If, at any time, you encounter resistance, stop the procedure.
- Remove the dilator and take another radiograph to determine the new location of the coin.
- If the coin remains in the esophagus, the patient can undergo another attempt at bougienage at the discretion of the provider. If still unsuccessful, you will need to contact your gastroenterology colleagues.
- If the coin is now in the stomach, the patient can be observed for a short time in the emergency department and then discharged home with detailed follow-up instructions.
Follow-up
Pages: 1 2 3 4 | Single Page





No Responses to “Bougienage Good Alternative for Treating Retained Esophageal Coins”