
Co-ingestion of a magnet with a button battery necessitates removal. After removal, some advocate for a delayed second-look endoscopy to ensure no damage has occurred. It is important to note that perforations and fistulas may develop up to 18 days after removal. Strictures can develop weeks and months after removal.
Explore This Issue
ACEP Now: Vol 33 – No 09 – September 2014Even though button batteries represent a genuine hazard, emergency physicians alert to the signs and symptoms of button battery ingestion can effectively manage them and help their patients achieve good outcomes.
Case 1
A 3-year-old male was well until he vomited bright-red blood and became unresponsive; EMS transported the patient to the hospital. He arrived in asystole cardiac arrest, with blood around his nose and mouth, and received continuous pediatric advanced life support. Despite this, he expired.
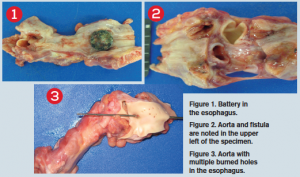
At postmortem, a button battery was found impacted in the esophagus at the level of the transverse aorta. There was a fistula connecting the esophagus and aorta, with the esophagus packed with bright-red blood and with gastric content of large dark-colored blood clots. The small and large bowels were also found to be packed with dark-colored stool.
Case submitted by Eugene Varghese, MD, Rutgers New Jersey Medical School in Newark, and David Woodkotch, MD, chief resident of emergency medicine at Rutgers.
Case 2
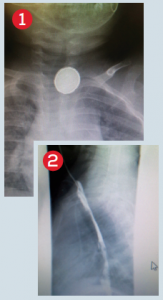
A 5-year-old female who was “playing around” with her grandma’s battery while hanging out in her grandma’s car ingested a button battery. She waited a few hours before telling anyone and was seen about six hours after ingestion. She complained of a sore throat and had no difficulty with secretions or breathing. Lateral and anteroposterior chest X-rays showed a battery lodged in her upper esophagus (see Figure 1).
We used propofol for endoscopy done by a pediatric gastroenterologist while in the ED. She was admitted by pediatrics after retrieval of the battery for concern of necrotic tissue in the upper esophagus noted by the gastroenterologist (see Figure 2). She was initially placed on antibiotics by us and steroids by the gastroenterologist out of concern for possible perforation and/or mediastinitis (which did not occur). Figure 3 shows the button battery after retrieval.
Case and photos submitted by Peter Chase, MD, PhD, assistant professor of pharmacy practice and science at The University of Arizona in Tucson.
Case 3
Pages: 1 2 3 | Single Page





No Responses to “Button Batteries a Swallowing Hazard for Children”