The best questions often stem from the inquisitive learner. As educators, we love, and are always humbled by, those moments when we get to say, “I don’t know.” For some of these questions, you may already know the answers. For others, you may never have thought to ask the question. For all, questions, comments, concerns, and critiques are encouraged. Welcome to the Kids Korner.
Explore This Issue
ACEP Now: Vol 37 – No 01 – January 2018Question 2: For pediatric patients with suspected appendicitis, can a normal C-reactive protein (CRP) rule out acute appendicitis?

shutterstock.com
A prospective study by Sengupta et al evaluated the diagnostic accuracy of white blood cell (WBC) count and CRP for acute appendicitis.1 This study included 98 patients, of whom only 20 were pediatric patients. The authors found that a combined normal WBC (lower than 11,000) and a normal CRP (less than 10 mg/L) demonstrated a 100 percent negative predictive value (NPV) in patients younger than 18 years of age. Separately, the sensitivities of an elevated WBC and elevated CRP were 85 percent and 65 percent, respectively, for diagnosing histologically proven acute appendicitis. The authors stated, “No patient with a normal white cell count and CRP needed appendectomy, and therefore, depending on other clinical criteria, these patients do not require admission to the hospital.”
That was a single study with a very small pediatric patient population (n=20 children), and a number of other articles would suggest a different conclusion. For instance, in a single retrospective cohort study from two separate institutions by Vaughan-Shaw et al that included 297 patients (both adults and children), 17 patients with histologically proven acute appendicitis would have been sent home if the exact same criteria for WBC and CRP as stated above were used.2 That’s 5 percent and 8 percent of the histologically proven appendicitis cases from the two institutions examined in that study.
That research included both adults and children. So what have pediatric-specific studies found? A recent prospective study by Zouari et al evaluated 292 pediatric patients with the combination of Alvarado score (see Table 1), CRP, and ultrasound.3 Alone, the sensitivity of CRP was 77 percent, so it is an ineffective test for diagnosing appendicitis. When combining a negative ultrasound (defined as a normal appendix or no appendix visualized) with an Alvarado score of less than 4 and a normal CRP, the NPV was only 92 percent, which is still not a great NPV. The NPV was even worse (73 percent) if the Alvarado score was 5–6. In the end, the negative CRP demonstrated poor diagnostic ability for acute appendicitis.
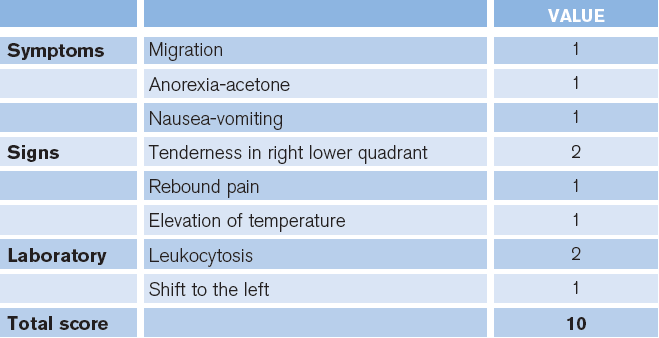
(click for larger image) Table 1. Alvarado Score for Diagnosing Acute Appendicitis
Credit: Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15(5):557-564.
In another prospective pediatric study by Benito et al, of 185 patients between 2 and 14 years of age, a CRP of less than 2 mg/dL demonstrated poor sensitivity (35 percent). Prada-Arias et al found a similarly poor sensitivity (43 percent) in a prospective study of 275 admitted children.4,5 These authors did not evaluate the combination of a normal WBC and normal CRP in these studies. With regard to a combined normal WBC and normal CRP, a retrospective pediatric-only study by Buyukbese Sarsu et al found that a WBC lower than 13,100 μL and CRP less than 1.17 mg/dL still missed six out of 278 (2.1 percent) cases of acute appendicitis.6
Summary
A normal CRP alone is an inadequate test to evaluate for acute appendicitis and should not change a practitioner’s suspicion of appendicitis by itself. In cases with a normal WBC and normal CRP, the literature suggests a lower likelihood of acute appendicitis, but these results do not rule out acute appendicitis.
 Dr. Jones is assistant professor of pediatric emergency medicine at the University of Kentucky in Lexington.
Dr. Jones is assistant professor of pediatric emergency medicine at the University of Kentucky in Lexington.
 Dr. Cantor is professor of emergency medicine and pediatrics, director of the pediatric emergency department, and medical director of the Central New York Poison Control Center at Upstate Medical University in Syracuse, New York.
Dr. Cantor is professor of emergency medicine and pediatrics, director of the pediatric emergency department, and medical director of the Central New York Poison Control Center at Upstate Medical University in Syracuse, New York.
References
- Sengupta A, Bax G, Paterson-Brown S. White cell count and C-reactive protein measurement in patents with possible appendicitis. Ann R Coll Sure Engl. 2009;91(2):113-115.
- Vaughan-Shaw PG, Rees JR, Bell E, et al. Normal inflammatory markers in appendicitis: evidence from two independent cohort studies. JRSM Short Rep. 2011;2(5):43.
- Zouari M, Jallouli M, Louati H, et al. Predictive value of C-reactive protein, ultrasound and Alvarado score in acute appendicitis: a prospective pediatric cohort. Am J Emerg Med. 2016;34(2):189-192.
- Benito J, Acedo Y, Medrano L, et al. Usefulness of new and traditional serum biomarkers in children with suspected appendicitis. Am J Emerg Med. 2016;34(5):871-876.
- Prada-Arias M, Vázquez JL, Salgado-Barreira A, et al. Diagnostic accuracy of fibrinogen to differentiate appendicitis from nonspecific abdominal pain in children. Am J Emerg Med. 2017;35(1):66-70.
- Buyukbese Sarsu S, Sarac F. Diagnostic value of white blood cell and C-reactive protein in pediatric appendicitis. Biomed Res Int. 2016;2016:6508619.
Pages: 1 2 | Multi-Page





One Response to “Can Normal C-Reactive Protein Rule Out Acute Appendicitis in Pediatric Patients?”
February 11, 2018
Dan MayerThe sample size wa way too small
The results of the pediatric group are data dredged as they are a subgroup of the whole study
Sensitivity and specificity are not given
The confidence intervals on the sensitivity and specificity are not given
Predictive values are only applicable in this population and should not be generalized