
A 28-year-old man presented with agitation. He was brought in by police and was restrained because of threats of biting and hitting police. The patient refused any additional medical care and stated, “I know my rights! You can’t hold me against my will.” When the emergency physician recommended vital signs, a history, and physical examination, the patient began hitting and biting staff, yelling obscenities, and threatening legal action. Should this patient be allowed to leave against medical advice (AMA)?
Explore This Issue
ACEP Now: March 02Leaving AMA
Informed consent and informed refusal of care are important components of patient autonomy, or self-determination, in medical decision making.1,2 Approximately 2 percent of emergency department (ED) patients in the United States leave prior to evaluation or AMA.3 Certain patient factors are associated with higher incidence of leaving AMA, including male gender, younger age, alcohol use, illicit substance use, weekend treatment, Medicaid insurance, and lack of medical insurance.4-6 Patients cite a variety of reasons for leaving AMA, including wait time, unmet expectations, anger, drug or alcohol use, family responsibilities, financial concerns, and negative interactions with staff.7,8
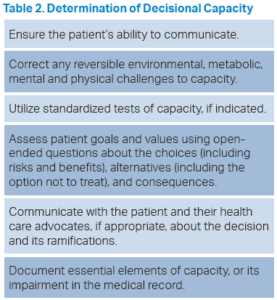
ACEP has summarized these issues in its Code of Ethics: “Emergency physicians shall communicate truthfully with patients and secure their informed consent for treatment, unless the urgency of the patient’s conditions demands an immediate response.”9 Patients with appropriate decisional capacity have the right to participate in the informed consent process and also have the right to refuse medical care. Informed consent and informed refusal are a process, not merely a signature on a form. Some erroneously believe that merely documenting a patient leaving AMA, using an “AMA form,” is sufficient to meet legal and ethical standards. The process of refusal of care, including leaving AMA, should include determination of decisional capacity, delivery of relevant information, including risks of refusing treatment, alternative treatments, and documentation of these elements. When a patient refuses medical treatment, care should specifically be taken to ensure that the patient understands the consequences, and that the physician expressed a willingness to treat the patient, including providing reasonable alternative treatments, and providing appropriate discharge instructions and follow-up recommendations (see table 1).
Patient Assessment
Assessment of capacity is an essential element of informed consent for treatment or informed refusal of care (see table 2).10,11 Multiple clinical conditions may impair capacity, such as cognitive disorders, neurologic disorders, medication effects, alcohol intoxication, substance abuse, psychosis, pain, anxiety, or any other condition that impairs ability to make an authentic choice.
Pages: 1 2 3 4 | Single Page






No Responses to “Can This Patient Leave Against Medical Advice?”