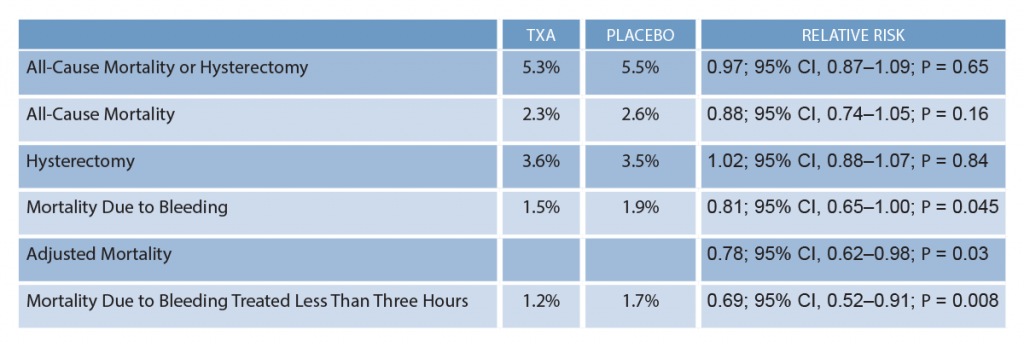
For the primary outcome of all-cause mortality or hysterectomy, there was not a statistical difference (see Table 1).
Explore This Issue
ACEP Now: Vol 37 – No 07 – July 2018EBM Commentary
1) Inclusion Criteria: The inclusion criteria in this study were vague. Clinical diagnosis of PPH was based on a subjective estimation of blood loss. Hemodynamic instability was not defined, and the clinician had to be unsure whether to use TXA.
2) Power Calculation: The trial was originally powered for a 25 percent relative reduction (1 percent absolute) in all-cause mortality or hysterectomy. After the trial started, they figured out the decision to do a hysterectomy usually was made at the same time as randomization. Therefore, they recalculated the sample size for a 25 percent relative reduction (0.75 percent absolute) in all-cause mortality. As a result, the sample size increased from 15,000 to 20,000.
Trials are often criticized for being underpowered but not for being overpowered. Trials are usually designed to find a difference between two things, and if you have a large enough trial, you will find a statistical difference because no two things are identical. Despite having more than 20,000 women, they did not find a difference in all-cause mortality.
3) Subgroup Analyses: A number of subgroup analyses for the primary composite outcome were considered a priori. The only statistical difference observed was if TXA was given in less than three hours postpartum. This result should be viewed with skepticism because subgroup analyses are considered hypothesis-generating and should not be overinterpreted.
4) Fragility of the Study: The fragility index is a way to measure the robustness of the results obtained.3 It is calculated by converting one patient (treatment or control) from a “non-event” to an “event.” In this case, how many women would have to have a different outcome for the study not to be statistically significant (P ≥ 0.05)?
This was a negative trial for the primary outcome of all-cause mortality or hysterectomy. However, there was a statistical difference in death due to bleeding. But the fragility index of this secondary outcome was zero, which emphasizes the lack of robustness of the WOMAN trial.4
The fragility index for the subgroup analysis of the secondary outcome of bleeding mortality treated in less than three hours is nine. This means if nine women switched from an event to a non-event in either group, the results of this hypothesis-generating result would no longer be considered statistically significant.
Pages: 1 2 3 | Single Page





No Responses to “Can Tranexamic Acid Decrease Maternal Mortality?”