
One component of this challenge that needed to be addressed included determining what services could be provided on an outpatient versus inpatient basis, thus freeing up capacity. In addition, there were a variety of different portals leading into the system. When a hospital is between 95 and 98 percent capacity, this can be extremely dangerous, especially with time-sensitive medical issues.
Explore This Issue
ACEP Now: Vol 36 – No 09 – September 2017Center Goals and Implementation
In 2011, the decision was made to create a centralized command center to address the access and throughput issues. With that decision, three core goals were established:
- Seamless entry of patients into the health system.
- Coordination of the safest, most appropriate transport of patients.
- Efficient management of hospital throughput needs.
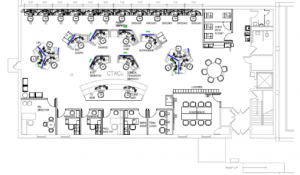
We were fortunate to be given the physical space previously occupied by the hospital library, which is a semicircle layout that works perfectly from a collaboration standpoint (see Figure 1). We worked with a space planner and were able to maximize the floor area to create strong partnerships between nurses and dispatchers as well as allow for the proper space for monitors and dashboards. Due to the success of the center and increasing needs, we are in the process of moving to a new, larger 4,400-square-foot off-site space (see Figure 2).
Engaging the staff was also a critical part of the implementation. Open communication, including having everyone who would be impacted involved in the planning, was an important first step. Transparent communications were also essential to overcoming other adoption challenges.
Benefits
The CTaC went live in 2012, and the benefits were felt almost immediately. First, it only takes one call to place a patient. The ability to have real-time capacity updates across all areas, in addition to being able to predict discharge dates based on historical data, had a positive impact on throughput and customer service.
The benefits were especially significant for the emergency department, which had been the biggest point of conflict, and include:
- Ability to see exactly how many patients are in the emergency department and where they’re going, making it possible to know if the department will be ahead on beds and staffing or needs to add more resources.
- Ability to instantly queue a helicopter to launch in order to transport a critically ill patient from a referring hospital.
- Real-time estimated time of arrival and patient updates during transport.
- Ability to launch preplanning before a patient arrives in order to make sure the hospital has the right bed type, leading to better overall outcomes as the right treatment starts sooner.
- Ability to provide the acceptance, as well as the mode of transport, thus removing the burden of transfer logistics.
Outcomes
The outcomes to date have also been significant:
- Eliminating 30 minutes of wasted time per patient means beds become available 30 minutes quicker and overall length of stay decreases.
- Using the metric of 1,900 admitted patients per month moving through the emergency department via the CTaC translates to approximately 60,000 hours saved per month to care for even more critically ill patients and 720,000 hours per year.
- Real-time emergency department alerts make it possible to precisely place patients and free up space to treat more people, resulting in a 50 percent reduction in the time it takes to place a patient in a room.
- There are year-over-year increases in transfer volumes, including a 40 percent increase in transfer admissions to the secondary campus.
- There is a decrease of 0.3 days in intensive care length of stay.
- The CTaC plays a central role in emergency operations and disaster management logistics at both the local and regional levels.
- The six dimensions of quality outlined by the Institute of Medicine are positively impacted.
- A real-time dashboard for senior leadership helps them monitor patient flow and make short- and long-term strategic decisions.
Conclusion
Providing exceptional care to patients and their families is at the heart of what we do—the CTaC helps us maximize our capacity to do that. By providing us with highly accurate real-time data, it enables us to drive systematic change at our organization.
Pages: 1 2 3 | Single Page





No Responses to “Carilion Clinic Transfer and Communications Center Helps Improve ED Patient Flow, Outcomes”