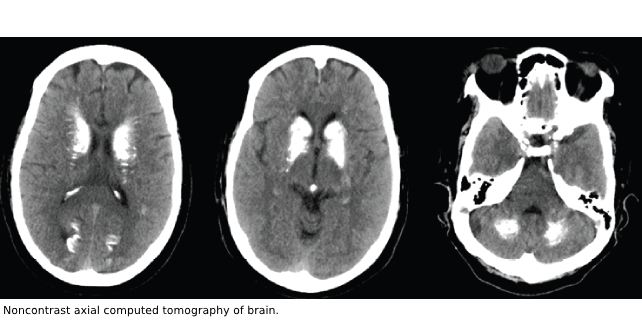
A 66-year-old woman presented to the emergency department (ED) after a witnessed seizure. On examination, the patient had mild confusion, a head laceration, and a tongue abrasion. She was noted to have a healed surgical scar present on the anterior neck. Images from the noncontrast computed tomography scans of brain are shown in the figure (right).
Explore This Issue
ACEP Now: Vol 42 – No 01 – January 2023Diagnosis: Extensive Brain Calcification Due to Hypoparathyroidism
The noncontrast computed tomography demonstrates extensive calcifications in the bilateral basal ganglia, periventricular white matter, and bilateral cerebellar hemispheres. Laboratory studies confirmed hypocalcemia: total calcium level was 4.6 mg/dL (reference range: 8.4–10.4 mg/dL) and ionized calcium was 2.65 mg/dL (reference range: 4.3–5.2 mg/dL). The patient had a remote history of a thyroidectomy and previous issues with hypocalcemia, but no prior seizures. Additionally, the patient reported not taking her prescribed calcium supplementation. While in the emergency department, she had another seizure. She received calcium gluconate and levetiracetam and was admitted to the medical intensive care unit (MICU). In the MICU, the patient received additional intravenous calcium gluconate, oral calcitriol, and calcium carbonate. Her parathyroid hormone intact level was 6.0 pg/mL (reference range 12.0–67.0 pg/mL).
Hypoparathyroidism leads to decreased serum calcium and increased serum phosphorus levels. The most common cause of hypoparathyroidism is iatrogenic from anterior neck surgery. Symptoms of mild to moderate hypocalcemia include paresthesias and tetany.1 Severe hypocalcemia can present as seizures, cardiac arrhythmias, broncholaryngospasm, and sudden death.1,2 Seizures with hypocalcemia are linked to increased neuroexcitability.3 The basal ganglia calcium deposition itself is not definitively linked to seizures.3,4
 Drs. Gombash, Bullard, and Frommelt are emergency physicians at the department of emergency medicine at Case Western Reserve University School of Medicine at MetroHealth Medical Center in Cleveland, Ohio.
Drs. Gombash, Bullard, and Frommelt are emergency physicians at the department of emergency medicine at Case Western Reserve University School of Medicine at MetroHealth Medical Center in Cleveland, Ohio.
References
- Clarke BL. Epidemiology and complications of hypoparathyroidism. Endocrinol Metab Clin North Am. 2018;47:771–782.
- John DR, Suthar PP. Radiological features of long-standing hypoparathyroidism. Pol J Radiol. 2016;81:42–45.
- Nageen T, Muhammad SZ, Jamal A. Seizures and basal ganglia calcification caused by hypoparathyroidism. Cureus. 2020;12(4):e7888.
- Zavatta G, Tebben PJ, McCollough CH, et al. Basal ganglia calcification is associated with local and systemic metabolic mechanisms in adult hypoparathyroidism. J Clin Endocrinol Metab. 2021;106(7):1900–1917.




No Responses to “Case Report: An Endocrine Enigma”