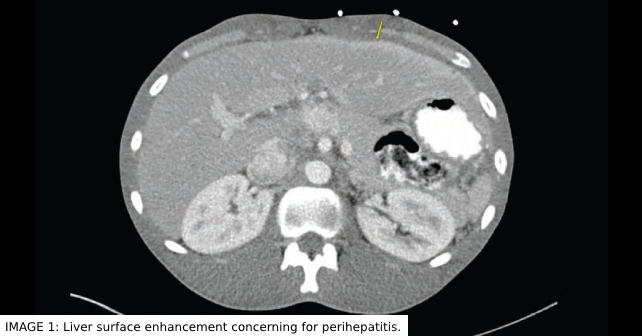
FHCS commonly presents with RUQ abdominal pain that can be pleuritic. It can be associated with fever, nausea, vomiting, headache, and overall malaise. In some cases, a friction rub may be auscultated along the right anterior costal margin. Liver enzyme levels and white blood cell counts are usually normal or slightly elevated, while erythrocyte sedimentation rate and c-reactive protein are often elevated.4 Since the clinical presentation of FHCS can mimic many other diseases localized to the RUQ, it is often mistaken for processes such as cholecystitis, hepatitis, acute pyelonephritis, or liver abscess. CT scan may show increased perihepatic enhancement or capsular thickening. However, direct visualization of perihepatic adhesions through laparoscopy is the only way to definitively diagnose. FHCS in men is exceedingly rare and possibly underrecognized.
Explore This Issue
ACEP Now: Vol 41 – No 12 – December 2022Discussion
There is a paucity of case reports of FHCS occurring in men. It is unknown if this is due to a lower prevalence of this complication, or just underrecognized. Case reports in men show a range of primary infections that led to FHCS. Urethritis, proctitis, and orchitis/epididymitis have been reported as initial pathologies prior to the formal diagnosis of FHCS.5,6,8,9 Given that there is no direct extension into the peritoneal cavity from these primary sites, unlike with direct extension from fallopian tubes in women, it is thought that hematogenous or lymphatic spread is responsible for the syndrome in men.8 Causative microorganisms are similar to those that affect women. Chlamydia and gonorrhea appear to be the most common organisms isolated in reported cases.5,6,8 Although definitive diagnosis is through direct visualization through laparoscopy, if there is a clinical concern, contrast-enhanced CT scan of the abdomen and pelvis is considered first-line imaging.9 Management of this disorder in men has not been thoroughly investigated. Antibiotic therapy should be pathogen directed, but when a pathogen is unknown and the patient requires admission, empiric therapy is warranted. We opted to treat as we would for PID in women—namely intravenous cefoxitin or cefotetan with doxycycline. With chlamydial sources, 21 days of doxycycline appears to be appropriate antibiotic management to treat this condition.8 However, when antibiotic management fails, direct lysis of adhesions via laparoscopy may be indicated for definitive therapy if symptoms continue.10
FHCS should be considered in any man who presents with worsening right upper quadrant abdominal pain or pleuritic right lower chest pain with recent or current symptoms of sexually transmitted disease such as urethritis, orchitis/epididymitis, or proctitis. Serologic testing for gonorrhea and chlamydia should be promptly performed and CT scan of the abdomen and pelvis can be utilized if clinical concern exists. Antibiotics with coverage against chlamydia and gonorrhea should be promptly initiated if a specific microorganism has yet to be identified. Patients should be informed that, if their abdominal pain does not improve with antibiotics alone, surgical intervention may be necessary.
Pages: 1 2 3 | Single Page





No Responses to “Case Report: Fitz-Hugh Curtis Syndrome in a Male with HIV”