
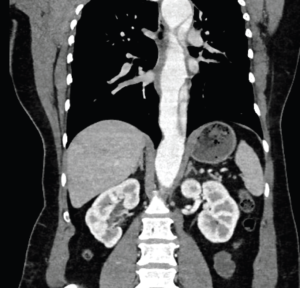
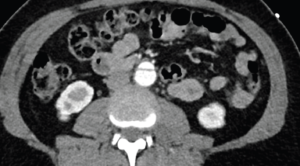
A 40-year-old woman with a history of untreated hypertension presented by ambulance after she was thrown from an ATV at unknown speeds and then crushed by the vehicle. The vehicle had no seatbelt or airbags, she was not helmeted, and she did not hit her head or lose consciousness. She reported 10/10 pain localized to her right arm and right flank, with no other complaints. On arrival, she was stable, airway breathing and circulation were intact, and Glasgow Coma Scale was 15. Initial vitals: HR 90, BP 161/142, RR 24, SpO2 100 percent on room air, afebrile. Primary survey was remarkable for an obvious deformity to the right forearm. Her secondary survey was remarkable for scattered abrasions and moderate bilateral flank tenderness. Her focused assessment with sonography for trauma was negative with bilateral lung sliding. The patient was neurovascularly intact throughout, with right upper extremity motion limited due to pain. Initial anteroposterior (AP) chest radiograph demonstrated no mediastinal widening, tracheal deviation, or pneumothorax. Plain film scout images of right upper extremity demonstrated a midshaft radius fracture.The CT scan of the chest, abdomen, and pelvis revealed a large traumatic Stanford type B aortic dissection. The patient was immediately started on esmolol and nicardipine drips with a systolic pressure goal of 120 mmHg. She was emergently transferred to a Level 1 trauma center by air ambulance, accepted by trauma surgery, and followed closely by vascular surgery.
Explore This Issue
ACEP Now: Vol 43 – No 07 – July 2024This case highlights the importance of recognizing concomitant trauma beyond a distracting injury. Traumatic aortic injury (TAI) is the second most common cause of mortality in non-penetrating traumatic injury; nearly 80 percent of cases die before hospitalization, and, of those who are hospitalized, mortality remains greater than 45 percent, with untreated mortality increasing one percent per hour.3,4 Most individuals suffering TAI are young males injured in motor vehicle accidents or falls.2 Although the most common originating site of a traumatic aortic dissection is distal to the left subclavian artery (LSA), in this case the proximal tear originated immediately upstream from the subclavian and distal to the left carotid artery.2 Plain radiographs of the chest may demonstrate findings of TAI—mediastinal widening, tracheal displacement, abnormal imprints of the aortic arch—but have low sensitivity and specificity, as reflected by normal findings in this case.2 The gold standard for imaging traumatic aortic injury is contrast-enhanced CT, with trans-esophageal echocardiogram being the second-best option if CT is not immediately available.2 Despite the ready availability of trans-thoracic echocardiogram (TTE) and its ability to capture aortic root dilation, cardiac tamponade, and dilation of the descending aorta and abdominal aorta, the sensitivity and specificity of TTE in traumatic aortic injury remains low and should not be relied on.2,3 In this case, aortic dissection was visualized neither on initial bedside nor on repeat inpatient TTE, despite operator knowledge of a known lesion and extensive operator training.
Treatment of the stable patient with TAI begins with blood pressure and heart rate stabilization, with pharmacologic management reducing risk of aortic rupture to less than two percent.3 Esmolol is the preferred medication for stabilization of aortic dissection and aortic aneurysm due to its pharmacokinetics and wide availability. Diltiazem, nicardipine, and nitroprusside should be considered as adjuncts.3 Of note, administration of nitroprussides before beta blockers can propagate aortic dissection due to the reflex catecholaminergic surge secondary to vasodilation, resulting in increased inotropy and downstream shearing forces on the aorta.4 To date, there are few evidence-based criteria for specific blood pressure goals in aortic dissection—ranging anywhere from 100 mmHg-140 mmHg systolic—although it has been shown that systolic blood pressure below 70 mmHg increases mortality.4 Meanwhile, guidelines for heart rate are more concrete, supporting optimization below 100 bpm, ideally 50-60 bpm.3,4
The cutoff for necessity of operative intervention beyond medical management is primarily determined by the grade of aortic injury as determined by CT angiography.3 Grade I involves intimal tear, Grade II involves intramural hematoma, Grade III is a pseudoaneurysm, and Grade IV is considered rupture; injuries rated Grade II and above are eligible for operative intervention.3 Morbidity, mortality, and risk of reintervention are decreased by medically temporizing patients for surgical intervention outside of the high-risk window: 24 hours of onset until two weeks from injury.1,3 Temporizing measures are not always possible for critically ill Grade IV patients, and outcomes are usually much worse.3 Fortunately, this case was found to be an uncomplicated Grade III dissection, which was determined to be safe for delayed endografting.
The patient stayed a total of nine days in the hospital and was discharged with a stable aortic dissection planned for future endovascular repair. Her orthopedic injury was managed non-operatively until her aortic repair could be performed.
 Dr. Arnot is a PGY-1 at the University of Arizona department of emergency medicine.
Dr. Arnot is a PGY-1 at the University of Arizona department of emergency medicine.
 Dr. Denq is an emergency physician at the University of Arizona department of emergency medicine.
Dr. Denq is an emergency physician at the University of Arizona department of emergency medicine.
References
- Huu AL, Olive JK, Cekmeceliouglu D, et al. Endovascular therapy for patients with heritable thoracic aortic disease. Ann Cardiothorac Surg. 2022;11(1):31-36.
- Mazzaccaro D, Righini P, Fancoli F, et al. Blunt thoracic aortic injury. J Clin Med. 2023;12(8):2903. Published 2023 Apr 17.
- Mouawad NJ, Paulisin J, Hofmeister S, et al. Blunt thoracic aortic injury–concepts and management. J Cardiothorac Surg. 2020;15(1):62.
- Sayed A, Munir M, Bahbah EI. Aortic Dissection: A Review of the Pathophysiology, Management and Prospective Advances. Curr Cardiol Rev. 2021;17(4):e230421186875.
Pages: 1 2 3 | Multi-Page




No Responses to “Case Report: Imaging Follows Dangerous ATV Accident”