A 29-year-old Hispanic American man with no significant medical history presented to the emergency department (ED) with a progressively worsening respiratory and systemic illness. His symptoms had begun two weeks prior, initially as a mild cough, congestion, and shortness of breath. About one week later, he started experiencing generalized body aches, nausea, and vomiting. By the day before his ED visit, his symptoms had worsened, and he developed new onset chills and muscle pain, which prompted him to seek care. He reported no recent travel outside of the country and no occupational or recreational exposures to arthropods or small mammals.
Explore This Issue
ACEP Now: Feb Digital 01-DOn arrival, he appeared diaphoretic and was in visible respiratory distress, with labored breathing and signs of acute discomfort. His physical examination revealed a punctate macular rash on his lower extremities and posterior thorax, which was initially thought to be nonspecific (see image 1). Given his significant distress, a comprehensive workup was initiated to rule out possible infectious, hematologic, and respiratory conditions.
A complete blood count (CBC), basic metabolic panel, hepatic function panel, urinalysis, respiratory viral panel, blood smear, ferritin, procalcitonin, erythrocyte sedimentation rate, C-reactive protein, blood cultures, and imaging studies were ordered. Imaging included a chest X-ray, CT angiogram (CTA) of the chest, and a CT scan of the abdomen and pelvis. Initial lab results revealed hyponatremia with a sodium of 130 mmol/L, and aspartate aminotransferase/alanine aminotransferase of 192, 140. His ferritin level was markedly elevated at 3,371.8 ng/mL, and his procalcitonin level was significantly increased at 6.84 ng/mL, both suggestive of a systemic inflammatory response. His CBC showed a low platelet count of 20,000/µL, mild anemia with a hemoglobin level of 12.1 g/dL, and a white blood cell count of 6.85 thousand/µL with a neutrophil predominance (92 percent) and the presence of smudge cells and schistocytes.
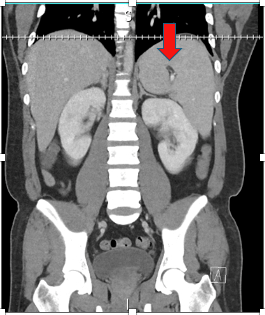
Image 3: CT abdomen and pelvis with IV contrast showing splenomegaly and splenic infarct. (Click to enlarge.)
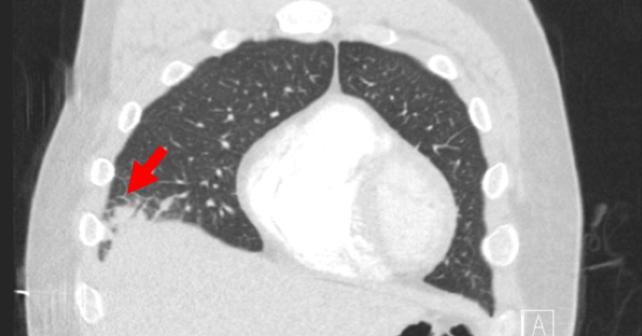
Chest CTA showed no evidence of pulmonary embolism; notable abnormalities included a right middle lobe consolidation consistent with pneumonia (see image 2), left ventricular dilation, interstitial pulmonary edema, and enlarged mediastinal lymph nodes. Abdominal CT revealed splenomegaly along with a splenic infarct (image 3). These findings collectively suggested a systemic inflammatory or infectious process with potential multiorgan involvement, but the specific cause remained unclear at this stage.
Pages: 1 2 3 | Single Page






No Responses to “Case Report: Murine Typhus Presents as Severe Pneumonia and Sepsis”