Many conditions outside of acute coronary syndrome (ACS) mimic ST-elevation myocardial infarction (STEMI), but only a handful of cases have reported ST-elevations (STE) in the setting of pancreatic inflammation where underlying ACS was excluded.1,2 While acute pancreatitis can involve electrocardiographic changes in up to 50 percent of cases, the exact mechanism causing STE remains unknown.3,4 Patients with ST segment elevation in the absence of classic ACS symptoms presents a dilemma for emergency physicians. Epigastric pain often raises concern for both cardiovascular and abdominal pathologies, including pancreatitis. Given the paucity of data and mechanistic uncertainty, a standard management protocol does not currently exist for patients with coexisting pancreatitis and ST segment elevation. Our case seeks to make emergency physicians aware of this phenomenon as recognition is essential in reducing patient exposure to unnecessary and potentially harmful interventions.
Explore This Issue
ACEP Now: Vol 42 – No 12 – December 2023The Case

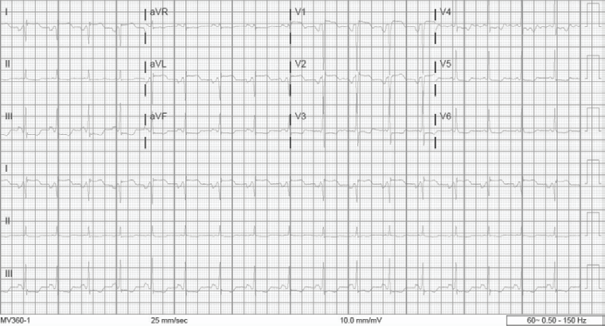
FIGURE 1: Initial EKG were notable for a leukocytosis of 23.19 k/uL, lipase of 87 U/L and an initial negative troponin of 3 ng/L HEART score of 1. The patient denied any chest pain or shortness of breath. A repeat ECG completed shortly after epigastric pain was controlled showed dynamic STE in aVL, V1 and aVR with diffuse ST depressions (see Figure 2). (Click to enlarge.)
A 60-year-old female presented to the emergency department with acute epigastric pain radiating to the back, nausea and vomiting. Pertinent medical history included atrial fibrillation with unclear adherence to apixaban, hypertension, peripheral artery disease status-post superficial femoral artery stent placement and chronic pancreatitis. The day prior to presentation, the patient was in her usual state of health and had been drinking wine coolers. Symptoms had been ongoing for nearly 22 hours prior to presentation. She was hypertensive and tachycardic with otherwise normal vital signs. On physical exam, she had epigastric pain to deep palpation without peritoneal signs or skin changes.
During the initial work-up, her ECG revealed STE measuring approximately 1 mm in V1, V2. There was also STE approximately 1 mm in I and aVL with diffuse ST depressions in the inferior leads, V3-V6 and aVR (see Figure 1).

FIGURE 2: Given concern for myocardial ischemia, cardiology was consulted and the patient was placed on ticagrelor and aspirin with transport arranged for emergent cardiac catheterization. Near complete pain control was achieved with a combination of nitroglycerin and morphine. During the delay to transport, a CT angiogram of the chest, abdomen and pelvis was completed and notable for peripancreatic acute on chronic inflammatory changes (see Figure 3). No evidence of pulmonary embolism, aneurysm or dissection was found. (Click to enlarge.)
Pages: 1 2 3 | Single Page




One Response to “Case Report: Pancreatitis Mimics STEMI”
December 31, 2023
Steven VAwesome work! very important to be aware of mimics in this field.