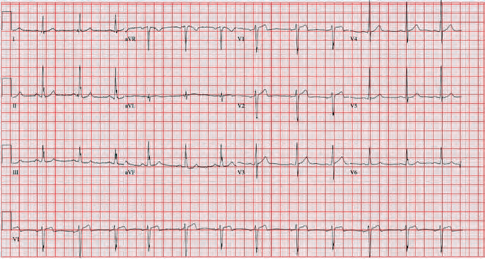
A 35-year-old male presented to the emergency department complaining of chest pain that started 1.5 hours prior to arrival. The patient had an EKG performed within 10 minutes of arrival while in triage (see Figure 1). In the absence of significant ST elevations, the EKG was signed and the patient was placed back in the queue to await a bed.
Explore This Issue
ACEP Now: Vol 43 – No 08 – August 2024Once placed in a treatment room, further history and physical examination are obtained. Two years prior, he had an NSTEMI requiring RCA stenting and is currently on dual antiplatelet therapy. He has prediabetes, hypertension, hyperlipidemia, and obesity. His vital signs were within normal limits. He appeared uncomfortable and slightly diaphoretic. His cardiopulmonary exam was unremarkable.
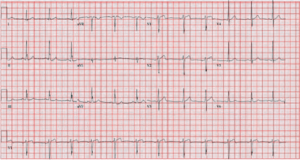
He was hospitalized two months prior and had a normal stress test. An EKG during that admission showed T-wave inversions in leads III and aVF (see Figure 2). These inversions have been present since his stent placement.
Diagnosis and Treatment
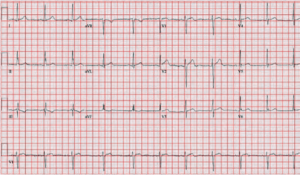
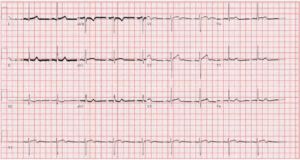
The patient was given aspirin, morphine, and nitroglycerin. He was pain-free and serial EKGs were performed showing a gradual return to his chronic inversion in lead III (see Figure 3). High-sensitivity troponins returned at 6 ng/L and 15 ng/L 1 hour apart (normal 0-20 ng/L). Given his EKG findings and presentation, he was started on heparin and admitted. His troponin peaked at 7,449 ng/L. One day after his initial presentation he was taken to the cath lab where it was discovered that he had severe in-stent restenosis of the RCA. He underwent balloon angioplasty with success and was subsequently discharged.
Discussion
The initial EKG performed demonstrated pseudonormalization of the T-wave in the presence of myocardial ischemia. Persistent T-wave inversions can occur for many different reasons such as underlying heart and pulmonary disease, persistent juvenile T-wave pattern, or for idiopathic reasons, amongst others. In the presence of ischemia, reversal of the inversions can occur. The relationship of this phenomenon to ischemia was first described in the 1970s in 38 patients where half displayed pseudonormalization of T-waves on stress test and half with anginal chest pain.1 The relationship was reconfirmed in several additional studies. It was later shown with continuous EKG monitoring that this process can occur when ischemia is present even in the absence of typical anginal symptoms.2
Pages: 1 2 3 | Single Page





No Responses to “Case Report: The Not So Normal, Normal EKG”