While there are many evidence-based guidelines and decision aids to guide imaging decisions in the emergency department (designed for indications ranging from pulmonary embolism [PE] to head injury), use of these tools is generally low. Even in the same hospitals, clinicians vary greatly in their use of imaging. As part of the ACEP Emergency Quality Network (E-QUAL), the avoidable imaging learning collaborative showcased “reducing avoidable imaging” success stories from emergency departments across the country.
Explore This Issue
ACEP Now: Vol 36 – No 08 – August 2017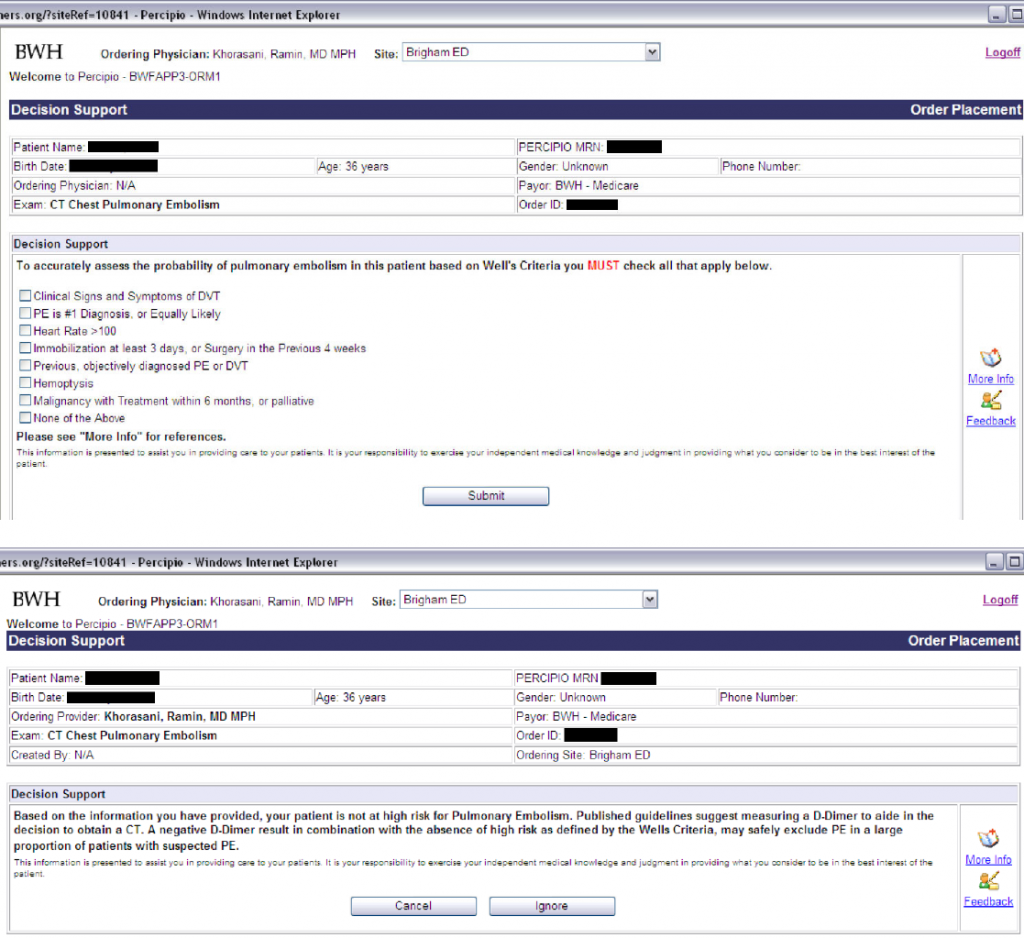
(click for larger image) Figure 1: (Top) Clinical decision support tool that provides automated calculation of the Wells score. (Bottom) Analysis of the calculated Wells score and its predetermined associated risk for pulmonary embolism.
Ali Raja, MD, MBA, MPH, executive vice chairman of the department of emergency medicine at Massachusetts General Hospital and an associate physician at Brigham and Women’s Hospital, both in Boston, led the development and implementation of several successful tools designed to improve guideline adherence for emergency department imaging. His team added real-time, evidence-based clinical decision support (CDS) to a computerized physician order entry system in order to improve adherence to best practices regarding ED imaging for PE. Figure 1 reflects how Dr. Raja and his colleagues implemented meaningful CDS that was nonintrusive, helpful to the clinician, and resulted in greater adherence with evidence-based practice. Figure 1 shows an automated calculation of the Wells score and feedback regarding the calculated score and its predetermined associated risk for PE.
What Did We Learn?
By integrating CDS tools and clinician variation feedback reporting, Massachusetts General and Brigham and Women’s hospitals have improved both the use of imaging and adherence to guidelines. In order to do this successfully, obtaining multidisciplinary leadership buy-in, including emergency medicine, radiology, internal medicine, and IT, while keeping in mind the main goal of always being patient-focused are important, Dr. Raja noted. “This means that we need to be sure to avoid imaging patients who don’t need it, but it also means that we should be imaging those who do,” he said. Improving the appropriateness of imaging required engagement of both inpatient and outpatient clinical service lines to ensure common clinical expectations because avoiding imaging in the emergency department does not do patients any good if they will get it anyway as soon as they are admitted.
Figure 2 reflects a not statistically significant decrease in ordered CT pulmonary angiography (CTPA) in hospitalized patients.

(click for larger image) Figure 2: Decrease (not statistically significant) in inpatient CT pulmonary angiography (CTPA) use. Red shows Month 31, 26.0 per 1,000 admissions. Blue shows Month 32, 22.8 per 1,000 admissions. Relative reduction was 12.8 percent (p=0.008). No significant increase or decrease in CTPA use trends observed (p=0.52). Data from Radiology. 2015;276(1):167-74. Credit: Ali Raja
Pages: 1 2 | Single Page





One Response to “Clinical Decision Support Tools Can Help Emergency Physicians Put Guidelines into Practice”
October 9, 2017
InferaYes, you’re right! A Clinical decision support systems provide real-time guidance to physicians on the appropriateness of diagnostic imaging tests for a given patient during the ordering process.