
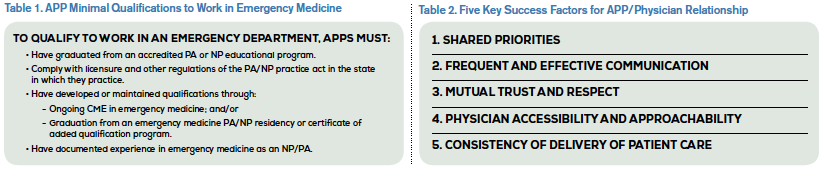
When recruiting an APP, an emergency department should consider its needs and match the expectations of the ED and the APP. Another aspect to consider is the level of experience (see Table 1). Any hospital or emergency medicine group hiring a new graduate should be mindful that a newly trained APP requires more mentoring and closer collaboration than an experienced APP. A seasoned APP with emergency medicine experience will be more likely to hit the ground running, may work at a more rapid pace than a new graduate, and may be able to handle a higher volume of patients.
Explore This Issue
ACEP Now: Vol 34 – No 02 – February 2015The next question is how to gauge ongoing competence. One method is to do a 360 survey. Such feedback can be a powerful tool for competency evaluation in a rapidly changing and often bewildering emergency medicine clinical environment. Of course, these tools must be used appropriately and intelligently in order to be effective. Here’s how it might work: All coworkers of a particular clinician would be surveyed on the perceived elements of clinical competence, including knowledge, application of knowledge, efficiency, ability to make decisions, and attitude toward patients. Every person in the emergency department could anonymously complete the survey. This would include nurses, techs, other APPs, housekeeping, on-call members of the medical staff—literally everybody, although not all of them will be capable of making some of these determinations. Then the ED director would let the clinician review and discuss the feedback. Everyone in the department would know they would be similarly evaluated.7 This is the most brutal, yet fair and efficient, way to assess competency in its broadest sense. Will all of the opinions be factually substantiated? No! What better technique do we have, at least for now?
But wait! Perhaps competence is not the endgame. Perhaps competence is really a minimum standard. Competence, albeit novice if we use the Benner model, is measured by completion of the PA or NP curricula (meeting the course objectives) and passage of board/licensure exams, just as physician competence is, essentially.
Most, if not all, would agree that mastery is achieved by the acquisition of additional knowledge (certificate of added qualifications, advanced certification) coupled with sound practice and experience. Mastery or expertise, some say, is what we should focus on, the achievement of which is quite individual. All clinicians can move toward mastery, but not all will actually achieve it. I suggest that competency is the starting point and mastery (expertise) is achieved by the ongoing commitment to expand clinical knowledge—keeping up with the literature, completing CME programs, learning from fellow clinicians—coupled with an extensive clinical experience in which knowledge is clinically applied with the achievement of the best results feasible within the constraints of the individual patient encounter.8
Pages: 1 2 3 4 | Single Page





One Response to “Competency Measurement Approach for Advanced Practice Providers in Emergency Medicine”
February 16, 2015
Gerry KeenanA timely explanation!We can only hope it guides reasoned decision making.