The Case
A 33-year-old female with a past medical history of anxiety presented to the emergency department complaining of back pain and right lower extremity weakness. The patient denied any recent illnesses, nausea, vomiting, fevers, or chills but reported three days of low back pain, recent onset of right lower extremity weakness, numbness, and tingling. She said that the weakness began suddenly, approximately 20 hours prior to ED arrival.
Explore This Issue
ACEP Now: Vol 39 – No 12 – December 2020On arrival, her temperature was 97.9°F, pulse 109 bpm, respiratory rate 20, blood pressure 130/90, and oxygen saturation 98 percent on room air. The physical exam revealed a nonambulatory alert and oriented, well-developed, well-appearing, anxious woman in no acute distress. The patient’s musculoskeletal exam was positive for midline tenderness on the lumbar spine located in the L4, L5 region. Neurologically, she had decreased strength (1/5) in the right lower extremity, with decreased sensation down her right lower extremity as well as diminished deep tendon reflexes. The left lower extremity was normal.
Upon further questioning, the patient reported an inability to void for 24 hours. A bedside ultrasound of her bladder demonstrated significant bladder distention. A Foley catheter was placed, and 1 L of urine promptly drained.
The patient was undressed for a detailed integumentary system exam, which did not reveal any insects, insect bites, or rash. All laboratory work was unremarkable and within normal limits. Neurology and neurosurgery were emergently consulted, and the patient was taken for immediate MRI without contrast of the brain, cervical spine, thoracic spine, and lumbar spine.
The MRI demonstrated expansion of the spinal cord, starting at C5 and extending to the T9–T10 level (see Figure 1). The MRI showed areas of hemorrhage in the spinal cord most prominent at the T2 level, with multiple serpentine structures consistent with a spinal cord vascular malformation (sAVM) (see Figure 2). The cord edema and expansion presumably reflected venous congestion/hypertension (see Figure 3). A neurosurgery consultation was obtained, and a catheter angiography was performed, localizing the lesion. At the choice of the patient and her family, the patient elected to transfer to another hospital.
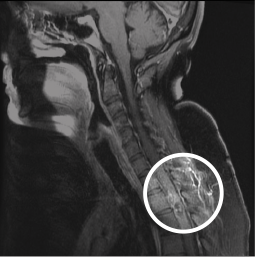
Figure 1: Cervical MRI showing expansion of the cervical cord, originating at the C5 level and extending into the lower thoracic spine. The most prominent areas of hemorrhage are in the T2– T3 levels, with multiple serpentine structures.

Figure 2: Thoracic MRI showing areas of hemorrhage in the spinal cord most prominent at the T2–T3 level, with multiple serpentine structures, most in keeping with a spinal cord vascular malformation such as an sAVM.
Discussion
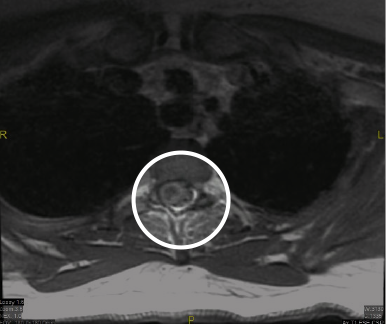
Figure 3: Thoracic MRI expressing cord edema and expansion, presumably reflecting venous congestion/hypertension. The cord appears to be scalloped due to dilated perivascular vessels.
Spinal cord arteriovenous malformations account for roughly 20 percent of all spinal masses and 3–4 percent of all space-occupying lesions in the spinal cord.1,2 The definitive diagnosis and treatment is to perform an angiogram with embolization (which has replaced digital subtraction angiography).1 Annually, about 300 patients in the United States present with an sAVM requiring hospital treatment, and the average length of related stays decreased from nine to six days between 1995 and 2006.3
Classifying sAVM type is essential to decide the best course of treatment (see Table 1).
The patient presented here was diagnosed with a type II sAVM: intramedullary AVM. These typically cause symptoms in patients in their third decade of life. The presentation can be similar as in this case, with sudden onset or loss of neurological function and pain below the level of the lesion.4 The cause of sAVMs is unknown, but it is postulated they might be genetic.5 Management of sAVMs depends on more than just the type or location but the ability and surgical experience of the neurosurgeon.
Table 1: AVM Types
| Type I | Spinal Dural Arteriovenous Fistula |
| Type II | Intramedullary AVM |
| Type III | Juvenile Malformations |
| Type IV | Intradural or Premedullary AVM |
Conclusion
Intramedullary sAVMs are a rare cause of acute neurological deficit and back pain that may present similarly to cauda equina syndrome. Although this patient did not suffer from cauda equina, all symptomatology that was appreciated by the patient fit the criteria for said pathology, which promoted the emergent imaging. Emergency physicians must identify and recognize this as possible cause of acute back pain. If any of the usual red flags for back pain are present, an MRI is recommended in conjunction with neurology and neurosurgery consultation. The emergency physician should make a quick decision for imaging to identify life- or function-threatening pathology.
Look for the following when evaluating a patient with back pain:
- Decreased sensation of the lower extremities
- Decreased muscle strength
- Perineal paresthesia
- Urinary or bowel incontinence/retention
Dr. Lopez is a second-year resident with the Emergency Medicine Residency Program at Good Samaritan Hospital Medical Center in West Islip, New York.
Dr. Schwartz is associate research director with the Emergency Medicine Residency Program at Good Samaritan Hospital Medical Center.
Dr. Smith is a board-certified emergency medicine physician at Good Samaritan Hospital Medical Center.
References
- Ozpinar A, Weiner GM, Ducruet AF. Epidemiology, clinical presentation, diagnostic evaluation, and prognosis of spinal arteriovenous malformations. Handb Clin Neurol. 2017;143:145-152.
- Endo T, Endo H, Sato K, et al. Surgical and endovascular treatment for spinal arteriovenous malformations. Neurol Med Chir (Tokyo). 2016;56(8):457-64.
- Lad SP, Santarelli JG, Patil CG, et al. National trends in spinal arteriovenous malformations. Neurosurg Focus. 2009;26(1):1-5.
- Yogarajah M. Crash Course Neurology. London: Elsevier; 2015:165.
- Kim H, Su H, Weinsheimer S, et al. Brain arteriovenous malformation pathogenesis: a response-to-injury paradigm. Acta Neurochir Suppl. 2011;111:83-92.





One Response to “Consider This When Evaluating Mysterious Back Pain”
January 3, 2021
Michael chandler md facepWhat treatment was offered this patient and what was outcome?