There are two causes of difficult airway: anatomy and physiology. These two factors are not always equally considered. Sometimes, difficult physiology is overlooked. This makes sense. You can’t just eyeball a patient’s physiological profile.
Explore This Issue
ACEP Now: Vol 39 – No 07 – July 2020This may be one reason the focus of difficult airway prediction has historically been on identifying anatomical challenges that interfere with direct laryngoscopy, commonly aggregated in the LEMON mnemonic (Look externally, Evaluate, Mallampati, Obstruction or obesity, Neck mobility).1 Over time, the focus of airway assessment expanded to include mask ventilation, extraglottic devices, and cricothyroidotomy, each with unique predictors of difficulty summarized in standard mnemonics from The Difficult Airway Course and the Manual of Emergency Airway Management.1
We’ve made great progress with this framework. As emergency airway management has evolved, the number of cases in which intubation cannot be rapidly achieved in the emergency department has shrunk to only a few percent. In fact, the rate at which surgical airways is performed is now less than 0.5 percent.2 There has been growing recognition that difficulty completing the procedural mechanics of intubation is only part of the challenge; studies demonstrate up to a 19.2 percent incidence of hypoxemia, 25 percent incidence of hypotension, and 4 percent to 11 percent incidence of cardiac arrest.3–6
While challenging anatomy may contribute to these complications, it is often the patient’s underlying physiology that has the greater impact. Success with the first attempt is associated with a dramatic reduction in complications, but a complication rate up to 20 percent is associated with physiological disturbances, which may be amenable to modification prior to intubation.7–9 From these experiences and observations evolved the distinct concept of the “physiologically difficult airway” to contrast with the “anatomically difficult airway.”10
The addition of an “S” to LEMON to make LEMONS was an early attempt to add consideration of a patient’s physiology to the preintubation assessment, but this only accounted for hypoxemia.11 Similarly, the HEAVEN mnemonic adds consideration of hypoxemia and blood loss to traditional anatomical markers.12 Other major physiological variables to be considered include increased oxygen consumption, right heart dysfunction, severe metabolic acidosis, and hypotension. We believe that the physiologically difficult airway deserves its own mnemonic, CRASH, to help recognize and modify the critical physiological variables in advance of intubation (see Table 1). CRASH can be used to remember the following considerations:
Table 1: The CRASH Mnemonic
| Physiological Abnormality | Response | |
|---|---|---|
| C | Consumption Increase | Optimize preoxygenation, apneic oxygenation; anticipate short apnea times |
| R | Right Ventricular Failure | Optimize preoxygenation, inhaled pulmonary vasodilators, choice of induction agents, early use of vasopressors |
| A | Acidosis (Metabolic) | Correct underlying issues; avoid mechanical ventilation, if possible; minimize apnea time/consider awake intubation; maintain increased minute ventilation |
| S | Saturation | Optimize preoxygenation, including noninvasive ventilation and DSI, apneic oxygenation, including high-flow nasal delivery |
| H | Hypotension/Volume | Volume resuscitation, vasopressors |
Consumption: The peripheral consumption of oxygen is increased in pediatrics, sepsis, acute respiratory distress syndrome, excited delirium, thyrotoxicosis, and pregnancy. These patients may exhibit a normal saturation during preoxygenation; however, the increased peripheral consumption may still result in rapid desaturation. Anticipating a shorter apneic time and maintaining adequate oxygen delivery to compensate for the increased consumption are of paramount importance. Any decreased oxygen delivery past the anaerobic threshold may lead to precipitous decompensation. Meticulous preoxygenation, improving low cardiac output, and correcting anemia may preserve adequate oxygen delivery.
Right Ventricular Dysfunction/Failure: In patients with right ventricular dysfunction, such as in massive pulmonary embolism, intubation is often the last step in the right ventricular “cycle of death.” The right ventricle (RV) has limited ability to increase contractility and output in response to increased demand.13,14 RV dilation and tricuspid regurgitation occur quickly when RV afterload is increased; this may be worsened by fluids administered in an attempt to increase the preload. Rapid sequence intubation paralysis may lead to hypercapnia, atelectasis, and hypoxemia, which all independently increase pulmonary vascular resistance and right ventricular afterload—often to the point of cardiovascular collapse. Cardiac ultrasound can help identify a failing RV and guide judicious fluid resuscitation, appropriate vasoactive, and inhaled pulmonary dilator medication use.10,13–15
Acidosis: Patients exhibiting profound metabolic acidemia, such as diabetic ketoacidosis, severe sepsis, or major trauma, present an increased risk because any interruption of ventilation or inability to match the necessary compensatory minute ventilation can result in life-threatening acidosis. A recent study showed that, with 60 seconds of apnea, pH drops 0.15 and PaCO2 increases by 12.5 mmHg, which can be devastating to fragile patients.16 Compensatory ventilation is best left intact by avoiding intubation, but if patients do require intubation, a strategy that limits or eliminates the apneic period and addresses the minute ventilation requirement postintubation should be adopted.
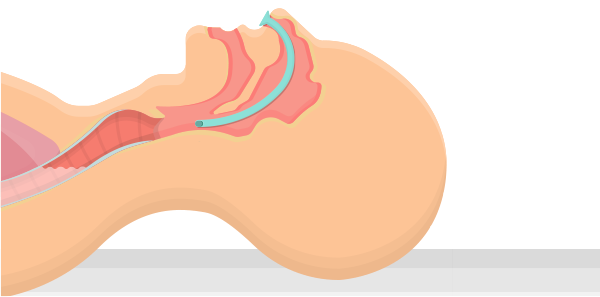
Saturation: Hypoxemia is a known complication of emergency airway management and has been associated with multiple complications, including peri-intubation cardiac arrest.3,6 Preoxygenation/denitrogenation are essential to assure maximal safe apnea time by providing a reservoir of oxygen to draw upon. Best performed with a tight-fitting mask and flush-rate oxygen, or a bag-valve-mask with one way valve and at least 15 liters of flow, denitrogenation may be objectively assessed by monitoring end-tidal oxygen.17 Upright positioning opens up functional residual capacity, while CPAP opens up functional residual capacity and recruits alveoli to improve ventilation-perfusion mismatch. In patients who will not tolerate CPAP, delayed sequence intubation (DSI) may be considered.18 In refractory hypoxemia, an awake intubation should be considered.19 Aerosol risk may also be considered for patients with COVID-19 and other highly contagious respiratory illnesses.
Hypotension/Volume: Critically ill patients requiring advanced airway management are at significant risk of hypotension in the peri-intubation period. Many critically ill patients are volume depleted or vasoplegic or have primary or comorbid cardiomyopathy. Induction agents and the transition to positive pressure ventilation can amplify these deleterious states and precipitate arrest. Fluid resuscitation, vasopressors, or inotropes may be indicated prior to intubation, depending on the clinical scenario.
The anatomically difficult airway is well-recognized and well-studied, although no faultless predictors exist. The physiologically difficult airway is equally important but generally underrecognized and underdiscussed. The CRASH mnemonic should assist in the assessment and management of the physiologically difficult airway. Addressing the factors represented in this mnemonic will help mitigate the risk of morbidity and mortality associated with advanced airway management in critically ill patients.
References
Pages: 1 2 3 | Single Page





One Response to “CRASH, a Mnemonic for the Physiological Difficult Airway”
December 27, 2020
Zameer Muhammadgood work by the team