Explore This Issue
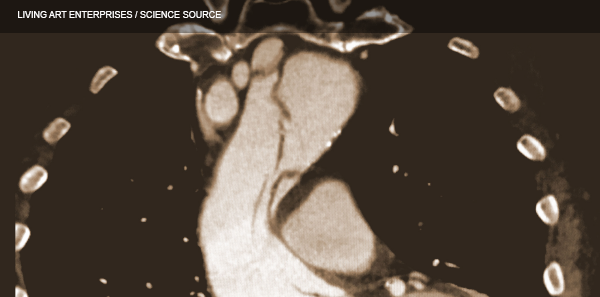
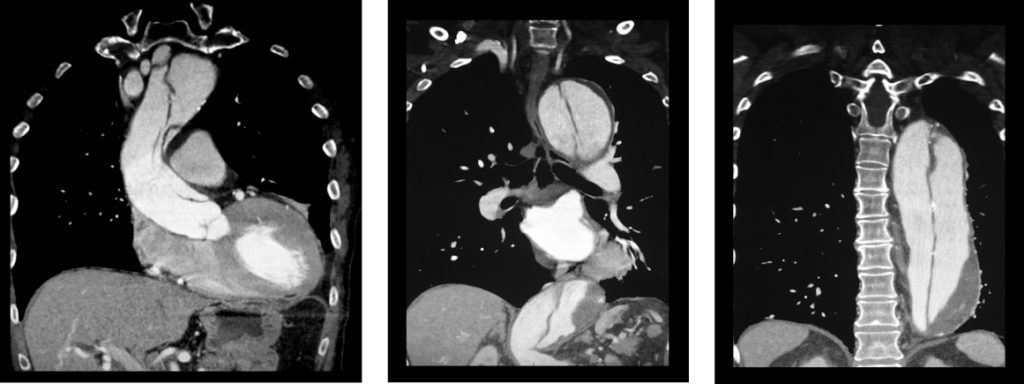
ACEP Now: Vol 36 – No 11 – November 2017(click for larger image) These three coronal reconstructions from contrast enhanced CT angiograms of the chest show an extensive dissection of the thoracic aorta. This is a De Bakey type I or Standord A aortic dissection.
Source: Living Art Enterprises / Science Source
In addition to thinking of CP +1, it may help to think backwards in time (1+ CP) and ask patients who present with end-organ damage if they had torso pain prior to their symptoms of end organ damage. For example, ask patients who present with stroke symptoms if they had torso pain before the stroke symptoms.
Anyone under the age of 40 years who presents to the emergency department with unexplained torso pain should be asked if they have Marfan syndrome. In the IRAD analysis of those under 40 years, 50 percent of the aortic dissection patients had Marfan syndrome, representing 5 percent of all dissections.1
- Look. The patient doesn’t always know they have Marfan syndrome, so you need to look for arachnodactyly (elongated fingers), pectus excavatum (sternal excavation), and lanky limbs.
- Listen. A new aortic regurgitation murmur has a surprisingly high +LR of 5.
- Feel. Feel for a pulse deficit, which has a +LR of 2.7, much higher than that of interarm blood pressure differences.
The patient’s blood pressure needs to be interpreted with caution and insight. Do not assume that the patient with a normal or low blood pressure does not have an aortic dissection. We know from the IRAD data that only about half of patients are hypertensive at initial presentation. Patients with aortic dissections that progress into the pericardium, resulting in cardiac tamponade, are often hypotensive. Patients with dissection who have a wide pulse pressure should be considered preterminal and usually require immediate surgery.
There is a lot more to chest radiograph interpretation for suspected aortic dissection than looking for a wide mediastinum. One-third of chest radiographs in aortic dissection are normal to the untrained eye, and a common pitfall is to assume that if the chest X-ray is normal, the patient does not have an aortic dissection. There are about a dozen X-ray findings associated with dissection, but two of them are especially important: loss of the aortic knob/aortopulmonary window and the calcium sign.
Look for a white line of calcium within the aortic knob, then measure the distance from there to the outer edge of the aortic knob. A distance >0.5 cm is considered a positive calcium sign, and a distance >1.0 cm is considered highly suspicious for aortic dissection. It is always wise to compare to an old film to see if there’s been an interval change.
Pages: 1 2 3 4 | Single Page





One Response to “How to Diagnose Aortic Dissection Without Breaking the Bank”
November 26, 2017
EricVery well written article on dissection. I especially like the thought process of thinking of it as the subarachnoid hemorrhage of the torso- really helps to remember those 3 questions.