Eighteen percent of patients with aortic dissection will have a positive troponin test, so if you suspect the diagnosis based on other clinical findings, don’t assume isolated acute coronary syndrome when the troponin comes back positive.5 Remember that fewer than one in 100 patients with a dissection will have associated coronary ischemia in any coronary distribution (most commonly inferior).
Explore This Issue
ACEP Now: Vol 36 – No 11 – November 2017While D-dimer seems like it might be appealing to help rule out the diagnosis in low-risk patients, for such a rare diagnosis and poor test characteristics of D-dimer for dissection, guidelines do not recommend the use of D-dimer for the workup of aortic dissection.6
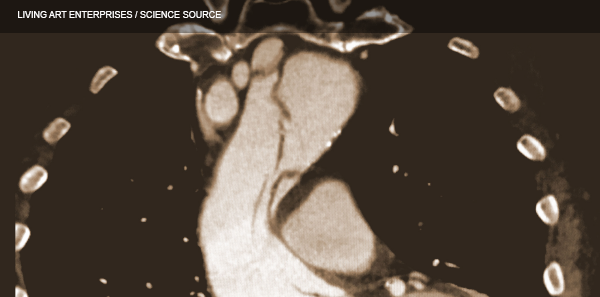
Aortic dissection can be considered the retinal detachment of the torso. While the sensitivity of point-of-care ultrasound (POCUS) by emergency physicians to detect an intimal flap is only 67 percent, the specificity has been shown to be 99 percent to 100 percent.7 For patients suspected of the diagnosis, look for an intimal flap that looks similar to a retinal detachment on POCUS and look for a pericardial effusion indicative of a retrograde dissection into the pericardium.8
Take-Home Points
- Remember the big pain pearls when taking a history:
- Ask the three important questions.
- Aortic dissection should be considered the subarachnoid hemorrhage of the torso.
- Migrating pain, colicky pain, plus need for IV opioids should raise your suspicion.
- Intermittent pain can still be a dissection.
- Look for Marfan syndrome, listen for an aortic regurgitation murmur, and feel for a pulse deficit.
- Think not only about CP +1 but also 1+ CP.
- Know the radiographic findings of loss or aortic knob/aortopulmonary window and the calcium sign, and use POCUS to look for an intimal flap and pericardial effusion.
- Don’t be misled by a troponin or D-dimer.
Thanks to David Carr for his expert contributions to the EM Cases podcast that inspired this article.
References
- Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283(7):897-903.
- Rosman HS, Patel S, Borzak S, et al. Quality of history taking in patients with aortic dissection. Chest. 1998;114(3):793-795.
- Imamura H, Sekiguchi Y, Iwashita T, et al. Painless acute aortic dissection: diagnostic, prognostic and clinical implications. Circ J. 2011;75(1):59-66.
- Singer AJ, Hollander JE. Blood pressure: assessment of interarm differences. Arch Intern Med. 1996;156(17):2005-2008.
- Leitman IM, Suzuki K, Wengrofsky AJ, et al. Early recognition of acute thoracic aortic dissection and aneurysm. World J Emerg Surg. 2013;8(1):47.
- Diercks DB, Promes SB, Schuur JD, et al. Clinical policy: critical issues in the evaluation and management of adult patients with suspected acute nontraumatic thoracic aortic dissection. Ann Emerg Med. 2015;65(1):32-42.
- Sobczyk D, Nycz K. Feasibility and accuracy of bedside transthoracic echocardiography in diagnosis of acute proximal aortic dissection. Cardiovasc Ultrasound. 2015;13:15.
- Fojtik JP, Constantino TG, Dean AJ. The diagnosis of aortic dissection by emergency medicine ultrasound. J Emerg Med. 2007;32(2):191-96.
Pages: 1 2 3 4 | Single Page






One Response to “How to Diagnose Aortic Dissection Without Breaking the Bank”
November 26, 2017
EricVery well written article on dissection. I especially like the thought process of thinking of it as the subarachnoid hemorrhage of the torso- really helps to remember those 3 questions.