Diagnostic testing options available to emergency physicians continue to expand. The conflicts over the use and cost of testing have spilled over into the popular press and have generated questions from the radiologists who provide many of the interpretations of the images ordered in the emergency department.1 Managing expensive diagnostic testing in the ED is one element of the value that emergency physicians bring to the American health system. It is important that all ED physician leaders understand the data on imaging rates to adequately address resource utilization queries and better manage their departments.
Explore This Issue
ACEP Now: Vol 34 – No 04 – April 2015The ED has a critical and growing role as the diagnostic center for the medical community. This role is particularly important for patients who are being evaluated for potential admission to the hospital due to an acute-onset injury or illness. Because 68 percent of inpatients are processed through the ED, emergency physicians are responsible for a disproportionate share of diagnostic testing and the patient-flow issues related to it.
Diagnostic testing has changed markedly over the last 20 years, with the advent of imaging technology using a broad range of modalities (ultrasound, ionizing radiation, magnetic resonance, positron emissions, etc.). These remarkable tools provide unprecedented ability to evaluate patients as they present with a wide range of clinical problems.
There are two sources of data related to the utilization of diagnostic imaging in the ED over the last decades. The Centers for Disease Control and Prevention (CDC) gathers and reports data through the National Hospital Ambulatory Medical Care Survey (NHAMCS). NHAMCS data from the CDC are available from 1992 through 2011, the last available year. The Emergency Department Benchmarking Alliance (EDBA) uses a voluntary data submission process from a large number of EDs and has collected and reported on data through 2013.
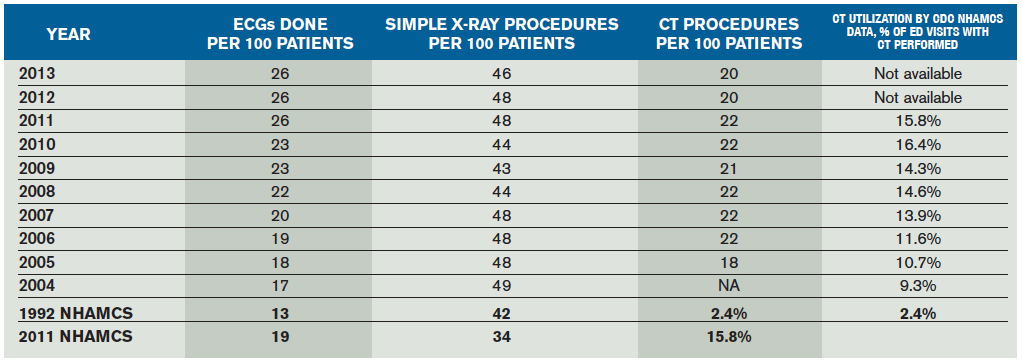
The NHAMCS data survey measures the percent of patients who receive an imaging study, not taking into account how many imaging procedures are done on any single patient. The NHAMCS report found that 44 percent of patients received a simple X-ray in 1992. In 2011, that number was only 34 percent. The NHAMCS report indicates that 2 percent of patients had CT scanning performed in 1992. This increased to 14 percent in 2007 and peaked at 16 percent for 2010 and 2011.
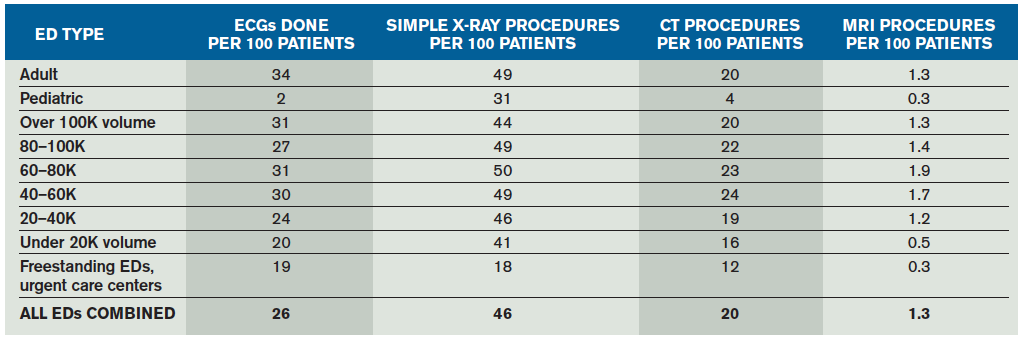
The EDBA reports on ED utilization of diagnostic imaging as measured in the number of procedures performed per 100 patients seen. A patient having multiple imaging procedures performed (eg, a hip X-ray and a chest X-ray) would have two procedures in the EDBA reporting system but only be credited as one imaging patient in the NHAMCS data. The EDBA data survey for 2013 was developed from the performance measures reported by 1,151 EDs that saw 45 million patients in that calendar year.2 The data are reported in cohorts based on type and volume of patients seen in the ED (see Table 1).
Utilization of CT scans appears to have peaked and has decreased during the last two years, based on the EDBA data surveys over the last 10 years (see Table 2). CT utilization peaked at 22 CT scans per 100 patients seen between 2006 and 2011. There was a 10 percent drop in utilization to 20 CT procedures per 100 patients seen in 2012 and 2013. This is consistent with a recent report that showed decreased growth in CT and MRI imaging rates over the last nine years.1
There is about a 50 percent difference in CT utilization based on ED volume, with the range between 16 and 24 procedures per 100 patients seen. Pediatric EDs only use CT imaging about four times per 100 patients seen. Plain diagnostic X-rays show little difference in utilization based on volume.
According to the EDBA report, MRI utilization across all EDs has now reached about 1.3 procedures per 100 patients seen, but this increases to 1.9 in the high-level trauma centers.
Trauma centers utilize diagnostic imaging to evaluate patients with critical injuries. Within the EDBA data set, the data have been sorted into separate cohorts of trauma centers (see Table 3). Pediatric trauma centers have very different profiles than general EDs, so they are excluded. The three cohorts are Level I and II trauma centers, Level III and IV trauma centers, and all other EDs.
Table 3 shows that the higher-level centers see patient populations with higher acuity, admission rates, emergency medical services (EMS) arrival, and longer time for processing. There are also differences in the use of diagnostics commensurate with the trauma level.
CT scans are used more frequently in Level I and II trauma centers than in lower-level centers. There are 26 CT procedures per 100 patients seen in Level I and II trauma centers and 18 to 20 procedures in lower-level and nontrauma centers. Emergency physicians in these EDs should be aware of the differences, and when called upon to study their utilization, they should compare their experience to cohorts at a similar level of trauma designation and pediatric mix.
It is critical that emergency physicians are able to use and understand the data on diagnostic testing in their department and have comparison data available for their peers. This will allow better decision making by all parties involved in utilization management.
 James J. Augustine, MD, FACEP, is director of clinical operations at EMP in Canton, Ohio; clinical associate professor of Emergency Medicine at Wright State University in Dayton, Ohio; vice president of the Emergency Department Benchmarking Alliance; and on the ACEP Board of Directors.
James J. Augustine, MD, FACEP, is director of clinical operations at EMP in Canton, Ohio; clinical associate professor of Emergency Medicine at Wright State University in Dayton, Ohio; vice president of the Emergency Department Benchmarking Alliance; and on the ACEP Board of Directors.
 Dr. Broida, is director of risk management for Emergency Medicine Physicians (EMP) in Canton, Ohio; is COO of EMP’s medical malpractice insurance company; and serves on the ACEP Medical Legal and EM Practice committees.
Dr. Broida, is director of risk management for Emergency Medicine Physicians (EMP) in Canton, Ohio; is COO of EMP’s medical malpractice insurance company; and serves on the ACEP Medical Legal and EM Practice committees.
References
- Arasu VH. Diagnostic emergency imaging utilization at an academic trauma center from 1996 to 2012. J Am Coll Radiol. 2015 Jan 23. [Epub ahead of print]
- The Emergency Department Benchmarking Alliance. Available at: www.EDBenchmarking.org.
Pages: 1 2 3 | Multi-Page






2 Responses to “Diagnostic Testing Usage Data Can Help Emergency Physicians Manage Utilization”
June 12, 2015
henry richterDrs. Augustine and Broida:
REF: “The ED diagnostic Center”, ACEP NOW April 2015
Your article brings up an interesting though subtle issue. Particularly focusing on soft tissues imaging ( US, CT, MRI), many of these tests are normal. The quick response is to bemoan the these normals as ” over-utilization”. However, the normals are of immense utility if used in the following manner.
Please be aware I am not an academic and these observations are based on a 36 yr medical career, half spent in ED care, and half in primary care.
Every normal test is predictive of remaining normal for a period of time. This infers that repeating the test will be de-facto over-utilization. The issue then is how long is this period of time? How much can this time interval be generalized to a population? How much of this time interval is specific to a single patient?
Let me give examples. A normal biliary ultrasound will remain normal, in the sense of the diseases of ED interest, for years. Two years at least, approaching five years in a younger cohort. A normal CT pulmonary angiogram essentially rules out any consideration of PE close to forever. Any PE that occurs in the years after a normal test must then immediately provoke a search for an underlying cause. A normal CT abd/pelvis is good for at least a year.
Of course clinical acumen is available, at any time, to over rule these generalizations. Cancer changes everything.
The statistics in your article do not educate me any any useful way. So what is my basic thought. However, I am presenting you with an opportunity to delve into barren numbers and attempt to find a teachable moment for providers. Will you design a study to track the stability of patients given certain imaging results? As our profession moves into the era of ACOs, the issues increases in importance.
Henry Richter MD
July 20, 2015
When the Hospital CEO Questions Test Utilization in the ED - THE FICKLE FINGER[…] has done a nice overview of the issue of the use of diagnostic testing utilization data in the ED, and this covers the issue in more […]