Myth #3: A Normal Physical Exam, Including Pelvic Exam, Can Rule Out Torsion
Up to one-third of patients have no tenderness on either an abdominal or pelvic exam.4–7,10 One of the key risk factors is an ovarian mass or cyst, but unfortunately, exams are also unreliable in detecting the presence of adnexal tenderness or mass, with an inter-examiner reliability ranging from 23 to 32 percent.5,30 Results are no better with a gynecologist-performed exam, with a sensitivity of detecting a mass >5 cm of 15 to 36 percent.5,31 The exam’s reliability further decreases in the setting of increased patient weight (defined as >200 pounds) and in patients older than age 55.32
Explore This Issue
ACEP Now: Vol 39 – No 06 – June 2020Key Point: A normal abdominal or pelvic exam does not exclude ovarian torsion.
Myth #4: A Normal Ultrasound Can Rule Out Torsion
Transvaginal ultrasound (TVUS) with grayscale imaging and Doppler flow is usually the go-to imaging modality to evaluate for torsion. While TVUS has high specificity, it has poor sensitivity, ranging from 35 to 85 percent.33–35 The most common finding is an enlarged ovary due to edema, often with a mass.5,16,17,33–36 Other signs include an ovary displaced to the midline. The “string-of-pearls sign,” in which an enlarged ovary is lined around the periphery by follicles, suggests torsion.5,16,17,33–36 Grayscale may demonstrate a hypoechoic appearance of the ovary due to edema. Color Doppler may reveal decreased or absent intraovarian venous flow, which may be followed by absent arterial flow later in the disease (see Figure 1).5,16,17,33–36 One major pitfall with TVUS use is reliance of normal arterial flow to exclude torsion, as the ovaries have dual blood flow from the ovarian and uterine arteries.5,34 Torsion initially occurs with lymphatic and venous outflow obstruction. Arterial inflow is not compromised until later in the disease course.35,36 Arterial flow is completely normal in more than 25 percent of patients with surgery-confirmed torsion, and more than half of patients will have detectable arterial flow.16,17,35,36 Therefore, assessing venous flow is a better indicator. However, intermittent or partial torsion may also result in normal venous flow TVUS.
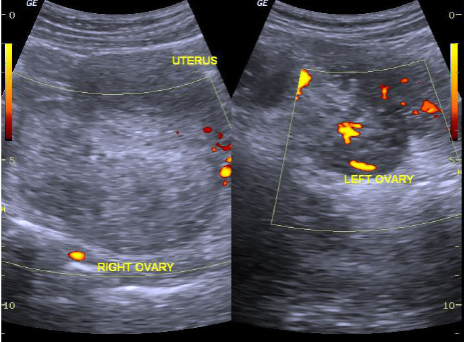
Figure 1 (ABOVE)
Ovarian torsion on ultrasound with enlarged ovary and absent vascular flow.
Case courtesy of Dr. Maulik S. Patel, Radiopaedia.org, rID: 30458
Literature suggests that combining ultrasound findings can improve sensitivity and specificity compared to only focusing on vascular flow.5 Evaluating for free fluid within the pelvis, ovarian enlargement and edema, and vascular flow can improve sensitivity.5 The whirlpool sign is strongly suggestive of torsion; it consists of a circular collection of blood vessels within an enlarged ovary or mass.5,37,38
Key Point: Do not rely on normal vascular flow to rule out ovarian torsion. A combination of TVUS findings such as ovarian enlargement and mass, free fluid in the pelvis, and vascular flow may improve your ability to diagnose ovarian torsion.
Pages: 1 2 3 4 5 | Single Page




One Response to “Dispelling 5 Ovarian Torsion Myths”
July 5, 2020
Jerry W. Jones, MD FACEP FAAEMExcellent article. Very concise and right to the point.