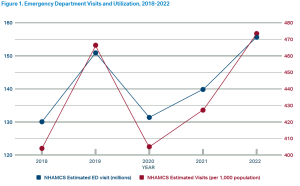
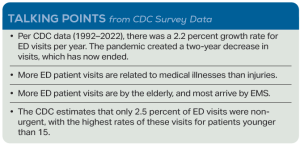
The Centers for Disease Control and Prevention (CDC) estimates of emergency department (ED) visits for 2022 were recently released.1 It was the highest volume ever reported by the CDC, at 155.4 million visits, with an all-time high utilization rate of 473 visits per 1,000 populations. This visit rate puts American EDs back on the data line it has followed since World War II.
Explore This Issue
ACEP Now: Vol 43 – No 12 – December 2024For quick comparison, ED visits in 2012 were about 131 million, which was 424 visits per 1,000 population. ED visit estimates and utilization rates for 2018 to 2022 are shown in Figure 1.
The CDC data are the oldest consistent data source for the United States, but the estimates of total ED visits remain different among the national data sources. This explanation has been published.2
Why the Increase?
Why are ED visits increasing? One significant driver of the increase is the aging population. Persons aged 75 and older had 660 visits per 1,000 population in 2021. In line with the aging U.S. demographics, EDs have provided excellent service to larger numbers of senior patients. Older patients typically have higher acuity than younger patients, which often means more diagnostics and treatment. Because older patients are admitted to the hospital more often, they disproportionately affect ED staff time and work.
The reality is that visits to EDs are the result of excellent service access. The patients and the community like the service provided in the ED, the availability of a wide range of diagnostic services, the immediate entrée to hospital admission, and the unfettered 24 hours a day/365 days per year availability. Almost half of ED visits are made between 5 p.m. and 8 a.m.3 In fact, when weekends are included, about 60 percent of ED visits are made outside of traditional business hours, which is becoming even more compressed in the post-pandemic years.
The ED is clearly perceived as serving the needs of patients and as the “front door to the hospital.” There is continuing growth in the percentage of overall hospital admissions presenting through the ED. The Emergency Department Benchmarking Alliance (EDBA) data survey found that about 69 percent of hospital inpatients are processed through the ED.4 The efficient ED processing of sick and injured patients, sorting the ones that would benefit from inpatient care, is a hallmark of high quality emergency care. But that efficiency is impeded by patient boarding.5
ED surveys done by the EDBA and the CDC report that there were more high acuity visits, senior patients, ambulance arrivals, diagnostic tests, and patients with mental health issues. Injury visits, which continue to decrease, now represent only 26 percent of visits.
Financial factors are stacked against patients getting service in the ED. Insurance companies have placed more and more financial penalties on patients who come to the ED, and charges by both hospitals and emergency physicians have escalated to produce high bills for these services. Nonetheless, the patients are still coming in higher numbers.
Quit Fighting the Market
A sensible approach would be to quit fighting the market—the many patients, families, and communities that want the ED to serve their acute, unscheduled care needs.
First, let’s work with hospital leaders to improve the efficiency of admitting patients and eliminate the boarding problems for patients admitted to the hospital. Let’s restore timely and patient-friendly patient transfer systems.6 Let’s develop a rational set of charges for care that match acuity and service delivered.
A critical need is for private insurance companies and government payers to follow payment policies that fairly pay emergency physicians. These policies should not be punitive to patients, with “no surprises” to the patient regarding their coverage for emergency services. Finally, service in the ED needs to be high quality and friendly to the 155 million patients and families—and growing—that sought us out in 2022.
 Dr. Augustine is a member of the ACEP Now Editorial Board, clinical professor of emergency medicine at Wright State University in Dayton, Ohio, and vice president of the Emergency Department Benchmarking Alliance.
Dr. Augustine is a member of the ACEP Now Editorial Board, clinical professor of emergency medicine at Wright State University in Dayton, Ohio, and vice president of the Emergency Department Benchmarking Alliance.
References
- Centers for Disease Control and Prevention. National Center for Health Statistics. Estimates of Emergency Department Visits in the United States, 2016-2022. Generated August 14, 2024. Accessed November 3, 2024.
- Augustine JJ. Emergency department patient challenges to come. ACEP Now. 2022;41(11):15.
- Coalition to Strengthen America’s Healthcare. 24/7 Access Makes the Difference: After-Hours Access to Emergency Departments Is Critical for Supporting Patients and Communities. Published July 29, 2024. Accessed October 31, 2024.
- Augustine JJ. Latest data reveal the ED’s role as hospital admission gatekeeper. ACEP Now. 2019;38(12):26.
- Augustine JJ. Long emergency department boarding times drive walkaways, revenue losses. ACEP Now. 2016;33(7):16.
- Augustine JJ. Interhospital transfer capabilities still pose major issues. ACEP Now. 2024;43(6):21.
Pages: 1 2 | Multi-Page



No Responses to “ED Volumes Keep Climbing as Patients Demand Acute, Unscheduled Care”