Summary
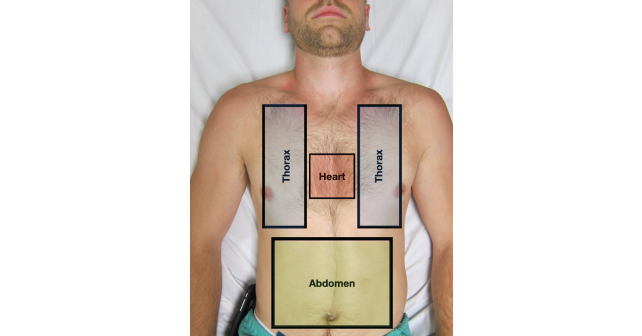
The eFAST examination has become a cornerstone of the evaluation of the critically ill trauma patient. The clinical context of the injury and hemodynamic status must be incorporated into the order and interpretation of the exam components. Utilize the “three box” concept as a framework and modify the order of the eFAST components depending on the mechanism of trauma and the patient’s clinical status. Proper and granular communication of ultrasound findings should be relayed to your trauma colleagues and interpreted in the hemodynamic clinical context of the patient. Finally, when faced with the newly or persistently hypotensive patient after an initially negative eFAST exam, a structured algorithm should be employed to reduce cognitive load in an often stressful situation. Our simple additions to the eFAST examination in no way replace the amazing work done by numerous physicians who have brought this life-saving tool into trauma care, but rather a minor refinement to an integral exam in modern trauma resuscitation.
Explore This Issue
ACEP Now: Vol 41 – No 09 – September 2022Dr. Leu is an ultrasound fellow at Highland Hospital.
Dr. Mantuani is the ultrasound fellowship director at Highland Hospital.
Dr. Sobrero is an ultrasound fellow at Highland Hospital.
Dr. Nagdev is director of emergency ultrasound at Highland Hospital.
References
- Rozycki GS, Ochsner MG, Jaffin JH, et al. Prospective evaluation of surgeons’ use of ultrasound in the evaluation of trauma patients. J Trauma. 1993;34(4):516–527.
- Kristensen JK, Buemann B, Kühl E. Ultrasonic scanning in the diagnosis of splenic haematomas. Acta Chir Scand. 1971;137(7):653–657.
- Montoya J, Stawicki SP, Evans DC, et al. From FAST to E-FAST: an overview of the evolution of ultrasoundbased traumatic injury assessment. Eur J Trauma Emerg Surg. 2016;42(2):119–126.
- Kirkpatrick AW, Sirois M, Laupland KB, et al. Hand-held thoracic sonography for detecting post-traumatic pneumothoraces: the Extended Focused Assessment with Sonography for Trauma (EFAST). J Trauma. 2004;57(2):288–295.
- Galvagno SM Jr, Nahmias JT, Young DA. Advanced trauma life support update 2019: management and applications for adults and special populations. Anesthesiol Clin. 2019;37(1):13–32.
- Gondek S, Schroeder ME, Sarani B. Assessment and resuscitation in trauma management. Surg Clin North Am. 2017;97(5):985–998.
- Press GM, Miller S. Utility of the cardiac component of FAST in blunt trauma. J Emerg Med. 2013;44(1):9–16.
- Bloom BA, Gibbons RC. Focused assessment with sonography for trauma. [Updated 2022 May 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan.
- Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Acad Emerg Med. 2010;17(1):11–17.
- Mandavia DP, Hoffner RJ, Mahaney K, et al. Bedside echocardiography by emergency physicians. Ann Emerg Med. 2001;38(4):377–382.
- American College of Surgeons Trauma Committee. Advanced trauma life support for doctors. 8th ed. Chicago, IL: American College of Surgeons; 2008.
- Friese RS, Malekzadeh S, Shafi S, et al. Abdominal ultrasound is an unreliable modality for the detection of hemoperitoneum in patients with pelvic fracture. J Trauma. 2007;63(1):97–102.
- Blackbourne LH, Soffer D, McKenney M, et al. Secondary ultrasound examination increases the sensitivity of the FAST exam in blunt trauma. J Trauma. 2004;57(5):934–938.
- Thomas B, Durant E, Barbant S, et al. Repeat point-of-care echocardiographic evaluation of traumatic cardiac arrest: a new paradigm for the emergency physician. Clin Pract Cases Emerg Med. 2017;1(3):194–196.
Pages: 1 2 3 4 5 | Single Page





No Responses to “eFAST 2.0: Refining an Integral Trauma Exam”