
Emergency department flow and reduction of patient walkaway are both very important performance measures. Flow requires coordinated utilization of staff, equipment, processes, and documentation. The Emergency Department Benchmarking Alliance (EDBA) has hosted three summits to develop the most effective definitions of time intervals and markers of care. The definitions are completed and published and are being used in the annual EDBA survey.1 The latest survey compiled 2013 data from 1,152 EDs that saw 45 million patients.
Explore This Issue
ACEP Now: Vol 34 – No 07 – July 2015The issues of timeliness of care, flow through the emergency department, and waiting room issues have clearly activated the regulators in the industry, the Joint Commission, and the public media. Patient flow includes the various intervals that reflect the time spent by a patient in the ED. A time interval is best expressed as an arithmetic median (the middle number of a set when the values are arranged in order from lowest to highest) as opposed to a mean (the average of a set of values).
ED leaders have most control over the flow of patients who are evaluated, treated, and released from the department. This represents about 80 percent of the patients seen in American emergency departments. ED staff can identify that the flow of patients who are ultimately admitted to the hospital, or transferred for admission to another hospital, is influenced by many factors outside their control. However, patients managed completely in the ED represent the overwhelming majority of the flow and also represent the persons more likely to express their displeasure with prolonged delays in care by walking out the door. For those who stay, longer delays (without explanation) are likely to result in lower scores on their experience of care.
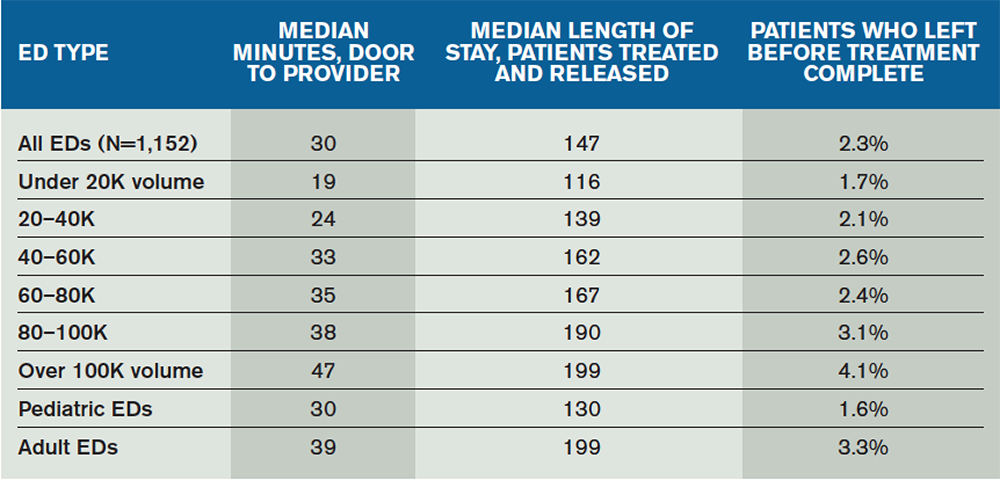
There is correlation between median length of stay and walkaway rates of patients from the ED (see Table 1). Within the cohorts of EDs, the patient population responds to flow improvements by reducing the tendency to walk away. Patient walkaway rates are particularly impacted by shorter “time to provider,” where the provider is either a physician or an advanced practice provider (APP).
The median time from door to provider for all EDs has decreased to about 30 minutes. The 10-year trend reflects that most EDs are improving the intake time, with clear stratification by ED volume. The EDs over 40,000 volume have a median time of about 37 minutes; that decreases to about 23 minutes for patients seen in EDs under 40,000 volume.
Pages: 1 2 3 | Single Page






One Response to “Emergency Department Flow, Patient Walkaway Key Performance Measures”
July 28, 2015
William WatkinsDid those EDs that place a provider in the intake system comment on how that provider is compensated for their work? If they are all salaried positions, it would not make a difference. Were there any groups placing a provider in the intake process that operated on a fee-for-service model? Did the improvement in efficiency cover the expense of placing a provider in a fee-for-service model in the intake process?