
The composition, demographics, and disposition of today’s emergency department patients are changing as quickly as the landscape itself, and this is changing how patients pay for EM services. Let’s see if we can connect the dots and get a better sense of the big picture using some of the most current industry information and data.
Explore This Issue
ACEP Now: Vol 35 – No 09 – September 2016Patient Experience Is Key
First and most important, in an article in Medscape, Nancy Melville documents the results from two European studies showing that “difficult” patients are frequently misdiagnosed.1 This is obviously most important for its medical-legal implications as well as its impact on patient experience. Wang and colleagues recently reported two significant findings based on the Centers for Medicare & Medicaid Services (CMS) five-star hospital rating system:2
- The number of stars was inversely associated with the risk-adjusted mortality rate.
- Hospitals with higher CMS star ratings were also associated with lower adjusted readmission rates, with five-star hospitals having the lowest readmission rate at 18.7 percent.
The take-home message for emergency physicians is, of course, to first stay totally focused on clinical issues. But it’s also important to be cognizant of the constantly building impact of patient experience-of-care issues and metrics. This is commonly a challenge, with some very sick or injured patients not being particularly open, nor receptive, to your best clinical intentions and actions. Additionally, the entire EM industry continues on its path toward increased commercialization of services: Kutscher reports that in March, HealthEngine offered patients up to $500 for having a preventive colonoscopy.3
Next, let’s connect a few more dots closer to home. Gooch reports that “74 percent of satisfied patients paid their medical bills in full, compared to 33 percent of their less-satisfied counterparts.”4 This is significant and important news for emergency physicians: Achieving high patient experience-of-care scores adds to the daily constraints and pressures in our emergency departments. This is especially the case in these days of an ever-increasing number of patients who are insured with high-deductible plans and the challenges incumbent on collecting from these patients.
Effects of Medicaid Expansion
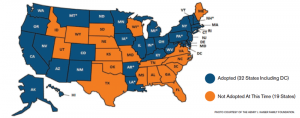
With this information as a backdrop, let’s examine the changes affecting emergency physicians currently occurring in the industry from Medicaid expansion. As seen in Figure 1, 32 states currently have expanded Medicaid.
What can Medicaid expansion mean for an EM practice? For an emergency department with an annual patient volume of 100,000 patients, the data are as follows:
Pre–Medicaid Expansion
- 100,000 annual patients
- Self-pay mix: 23 percent (23,000 patients)
- Self-pay cash/visit: $25
Pre–Medicaid expansion collection revenue:
- $575,000 annually Post–Medicaid Expansion
- Self-pay to Medicaid coverage movement of 18 percent (18,000 patients) at $60/visit ($1.08 million)
- Residual self-pay patients 5 percent (5,000 patients) at $12/visit ($60,000)
Post–Medicaid expansion collection revenue:
- $1.14 million annually Bottom Line Impact of Medicaid Expansion
- Total collections pre–Medicaid expansion ($575,000) versus post–Medicaid expansion ($1.14 million)
- Financial impact of Medicaid expansion: +$565,000 collection revenue
Notice the secondary finding of post–Medicaid expansion: Self-pay patient collections can be “less” than your practice’s prior self-pay collections. These are most likely your true self-pay patients—your residual self-pay patients who have not been absorbed into a Medicaid plan. Of related importance, however, is that Dussault et al reported early evidence that Medicaid expansion is fulfilling the goal of health insurance providing “peace of mind” by protecting against financial hardship.5 This certainly bodes well for patient experience-of-care scores.
Examine the Details
When looking at the connected dots thus far, it brings into focus the incredible significance of staying centered on your patient’s clinical presentation, coupled with the necessity of being supported by a business partner equipped with the latest analytical tools to efficiently drill down into the patient demographics and propensity-to-pay metrics. It also highlights the absolute necessity that the ED registration staff obtains accurate and current patient demographic information.
Pages: 1 2 3 | Single Page





One Response to “Emergency Department Patients’ Demographics, Disposition, Composition Affect How They Pay for Services”
September 25, 2016
Myles Riner, MDJohn, as I have said before, these kinds of calculations don’t take into account the possibility that newly insured Medicaid patients may use the ED more frequently than these enrollees did prior to having insurance coverage. The data is still a bit conflicting on this
https://www.macpac.gov/wp-content/uploads/2015/01/MACFacts-EDuse_2014-07.pdf
but it is likely to be driven by local conditions, such as the availability of primary care services for these new Medicaid enrollees. It is likely that in many areas where Medicaid expansion ensues, EDs and ED physician groups will find themselves having to staff up (and thus increase their overhead) to meet this demand, and since Medicaid almost always fails to cover the costs of providing these ED and emergency physician services: the net effect of Medicaid expansion for certain EDs may actually be a reduction in net revenues, rather than a gain. Arguments to the contrary just feed into the notion that the solution to ensuring the financial wellbeing of the emergency care safety net is to expand Medicaid. This may help some EDs and EP groups, or it may sink them, depending on circumstances often beyond their control (unless it forces them to skate around the thin ice of EMTALA violations by aggressively ‘deferring’ ED care of Medicaid patients).