Creation and Use of Training Model

Explore This Issue
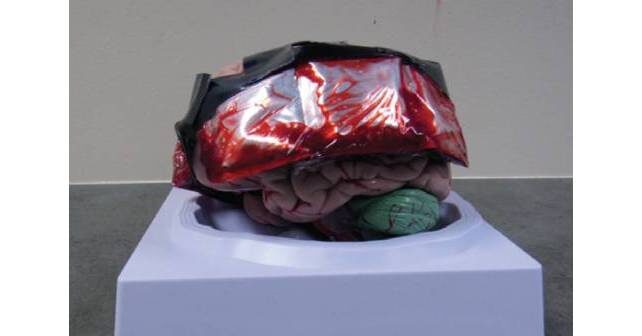
ACEP Now: Vol 41 – No 10 – October 2022FIGURE A: Brain model obtained from Amazon.com—$41.99.
In order to facilitate training, we first used the Galt trephine on an embalmed cadaver model. However, we learned that it required significant effort and time to enter the epidural space on the cadaver. Additionally, we recognized that the cadaver model was limited in availability and portability as a training model for physicians. So, this led to conceptualizing the simple, inexpensive model described below. Further, we were able to utilize the model as a procedural trainer in a recent mass casualty incident training exercise at Rocky Vista University College of Osteopathic Medicine in Parker, Colorado.
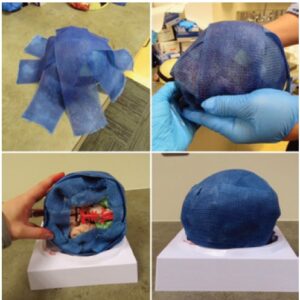
The model we created is constructed of a model brain (Figure A), an ice pack (evacuated of fluid and injected with simulation blood), cling wrap, tape, 3-inch-wide fiberglass casting material, and a repairable, simulation skin wrap.
The ice pack segments are drained of their fluid with an 18G needle and 10-cc syringe. Simulation blood, which can be commonly purchased online, is mixed with water to approximate the consistency of real blood and is then injected back into the segments using the same 18G needle and 10-cc syringe (Figure B). Each segment holds approximately 8 cc of simulation blood. The three continuous ice pack segments are then wrapped with cling wrap and secured to the brain model bilaterally in the temporal regions using strong adhesive tape (Figure A). Fiberglass casting material is molded around the model and blood packets to create a simulated skull, as seen in Figure C. After the fiberglass has dried and hardened, the repairable, simulation skin is wrapped around the skill model (Figure D).
This model results in a burr hole procedure that can be reproducibly performed. The model can provide physicians with a safe way to develop knowledge and muscle memory of a low-volume, high-risk procedure that would otherwise be typically left to didactic instruction and in-the-moment training.
We employed this model during the mass casualty incident training at Rocky Vista University College of Osteopathic Medicine. Medical students were provided a patient case presenting with an expanding epidural hematoma, as identified by signs and symptoms (initial loss of consciousness with lucid interval, followed by rapid decline in Glasgow Coma Scale and ipsilateral fixed and dilated pupil) and a provided CT scan image depicting an epidural hematoma. Once the indications for the burr hole procedure were recognized by the student, and the “patient” appropriately sedated and intubated, the model was provided to perform the burr hole (Figure E).
Pages: 1 2 3 4 | Single Page






No Responses to “Emergency Department Trephination (Burr Hole) for Epidural Hematoma”