Editor’s Note: The ACEP Council hosted a Town Hall meeting on mergers and acquisitions on Oct. 24, 2015, in Boston. Here is an edited transcript of the discussion, including the introduction by then-Council Speaker Kevin M. Klauer, DO, EJD, FACEP, chief medical officer–emergency medicine, chief risk officer for TeamHealth, and ACEP Now medical editor-in-chief.
Explore This Issue
ACEP Now: Vol 35 – No 01 – January 2016Introduction
Kevin Klauer, DO, EJD, FACEP
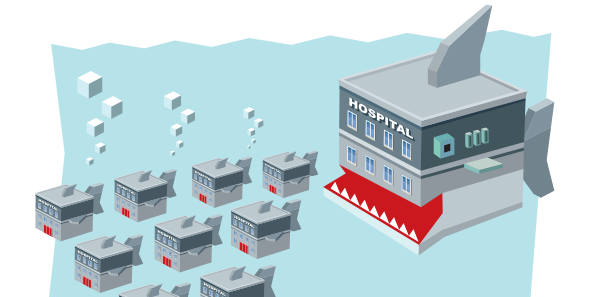
This is our Town Hall meeting and should represent a topic that is really important to the practice of emergency medicine, our specialty, and beyond: mergers and acquisitions. Many of us may not know a lot about this process and how it could impact us, but I think it’s time we discussed it so that we are all more informed about mergers and acquisitions in medicine. That’s why I titled this “Mergers and Acquisitions: The Medical Shark Tank.” I tried to get Mark Cuban; he still hasn’t responded to the request. I’ve asked Ricardo Martinez, who has a wealth of broad health care knowledge, to moderate this session.
Moderator

Ricardo Martinez, MD, FACEP, chief medical officer for North Highland Worldwide Consulting and assistant professor of emergency medicine at Emory University in Atlanta.
Participants

Brent Asplin, MD, MPH, FACEP, chief clinical officer for Mercy Health in Ohio
Savoy Brummer, MD, FACEP, vice president of practice development at CEP America in Belleville, Illinois, and chair of the ACEP Democratic Group Section
Ray Iannaccone, MD, FACEP, president of EmCare
Jay Kaplan, MD, FACEP, President of ACEP; director of the patient experience for CEP America in Emeryville, California; and a practicing clinician in the emergency department at Marin General Hospital in Greenbrae, California
RM: I think we have a very good group to talk about mergers and acquisitions, which are happening fairly quickly. The United States is seeing a lot of consolidation in many different markets. I’ll start with Dr. Asplin: what is driving hospital consolidation, and is that a good thing or a bad thing?
The first thing to consider is that, relative to other industries, we’re actually on the front end of a consolidation movement. We’re really still quite fragmented in health care. The majority of primary care practices in the country are still using three providers or less. Look at other industries, like how many U.S.-based global airlines there are now. Look at telecommunications, and soon we may only have three large for-profit health insurers that are national in scope. There are three basic financial drivers: liquidity and balance sheet drivers, operational metrics, and purchasing power. It’s about spreading fixed overhead costs to a larger base and gaining efficiency. It’s about building a stronger balance sheet to be able to withstand shocks to that balance sheet. Even though the cost of capital is at a historical low, it’s also about maintaining a strong rating to be able to access capital at rates that are favorable. You also want purchasing power in terms of supply chain and some asymmetry of negotiations. Those are the financial drivers, but I think uncertainty is one of the biggest drivers of consolidation. Even if all is going well for an independent community hospital, things can go from strong performance to the brink of solvency quickly, particularly with the dramatic swings we may be seeing in reimbursement. That is why you are going to see more hospital consolidation unless you have a compelling brand where you can continue to go at it as a single institution. Children’s hospitals would be some of the classic examples of a single-institution compelling brand. I think consolidation is a good thing for the system overall because we will lose fewer access points in hospitals because of it than we would if those hospitals remained independent.
Pages: 1 2 3 4 5 | Single Page





No Responses to “Emergency Medicine Leaders Discuss Drivers of Hospital Consolidation at ACEP15 Council Town Hall”