RM: Great, thank you. Two things to throw on your plate: one of those is a business concept called rule of threes that comes out of a Georgia Tech business school. Basically, everything consolidates down to three. Look at cellular companies. You mentioned the insurance companies consolidating to three. Secondly, everyone’s figured out it is time to go after the children’s hospitals, so they are under great stress right now. Savoy?
Explore This Issue
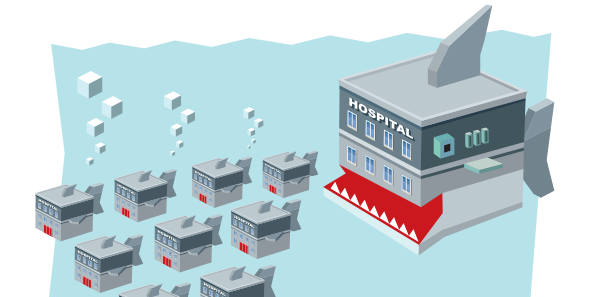
ACEP Now: Vol 35 – No 01 – January 2016SB: I would completely agree with all those drivers. I think uncertainty has another more common name, which is fear, and a lot of hospital systems have a fear of obsolescence. They’re looking to consolidate to eliminate much of their competition in other areas. They’re looking for new sources of revenue to, perhaps, offset some of their losses in other areas. Obviously, increasing their market share allows them to do that.
RM: Thank you very much. Dr. Iannaccone, in your role, you have a large perspective across the country.
RI: The only thing I would add is that as hospitals and health systems are looking at what they have to do over the next few years to maintain what thin margin they have, a small community hospital looks at the daunting task in terms of IT, purchasing, upkeep, or putting together a robust physician network. I think they recognize they need a certain amount of scale to do that. I’ve been told by health system CEOs that they know that the number of patients admitted to their hospitals is going to go down. They’re going to need a bigger, broader base of people to fill the beds while they’re in the gap years until they’re getting paid for quality.
RM: Thank you. Jay?
JK: Well, the single biggest driver of health care reform is cost. As organizations look to decrease their expenses, two of the ways they do that is to eliminate competition and to eliminate unnecessary expenses. One of the ways they can eliminate those items is through purchasing power, which Brent mentioned. Another strategy is to develop what are being called HROs, or highly reliable organizations. You can’t have 15 doctors with each wanting to do things their own way. You have to figure out what’s the one “our way.” When I was chief of emergency medicine for a 10-hospital health care system, we looked at the number of antibiotic prescribing regimens we had for community-acquired pneumonia; we had 37. By narrowing it to 10, we were able to save the system a couple of million dollars. I think that’s what organizations are doing as they are merging. They are looking to develop more consistency across all their different facilities and, by doing so, they reduce costs.
Well, the single biggest driver of health care reform is cost. As organizations look to decrease their expenses, two of the ways they do that is to eliminate competition and to eliminate unnecessary expenses. —Jay Kaplan, MD, FACEP
RM: Let’s turn it to emergency group consolidation. I wanted to separate those because they are two different things. I’ll ask the same question, and I’ll start with Jay. What’s driving that emergency group consolidation, and is that a good thing or a bad thing?
Pages: 1 2 3 4 5 | Single Page





No Responses to “Emergency Medicine Leaders Discuss Drivers of Hospital Consolidation at ACEP15 Council Town Hall”