RM: Great. Savoy?
Explore This Issue
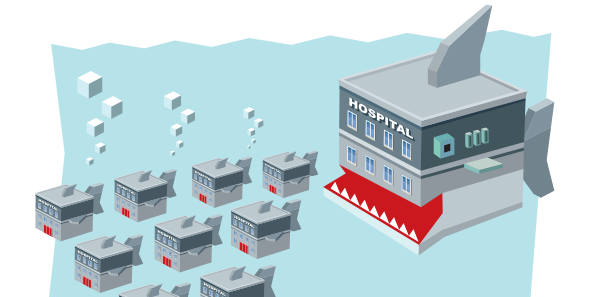
ACEP Now: Vol 35 – No 01 – January 2016SB: I think ideally most people would look at consolidation among professional services in a positive way if you are going to improve overall performance for patient care, if you’re going to improve the patient experience, and lastly, if you can do so in a setting maintaining or decreasing the cost curve. However, the majority of times we’re seeing many groups, especially independently owned groups, consider consolidation because of a failure, at least a perceived failure, of their ability to compete in the marketplace. I think, again, that there’s a large amount of fear from the eyes of the smaller independent groups. Lastly, I do believe that there’s a generational component in which there are many folks around retirement, and they’re looking for different means to monetize their practice. If you look at how Wall Street and private equity have subsequently performed after many of those acquisitions, you’ll see that performance hasn’t necessarily been ideal. I know that within my particular democratic group, we see over 5 million visits a year, but $100 million of our annual revenue comes from private equity or publicly held practices that had ultimately failed.
RM: Thank you. Dr. Asplin?
BA: I’m going to answer this from a hospital system perspective. We have 23 hospitals in seven markets across Ohio and one market in western Kentucky. Many of you are familiar with W. Edwards Deming, one of the most important quality-improvement process engineers of the 20th century. One of my favorite quotes of his is, “Uncontrolled variation is the enemy of quality.” I don’t know what the right answer is in terms of the right number of groups for a system like ours to work with, but I know it’s not 23 different groups. The answer, at least for the near term for us, isn’t to employ everyone, but we can’t work and get to scale fast enough if we have too many partners to work with. From a hospital system perspective, how can we get at the next level of quality, safety improvement, and cost reduction? I don’t care what the payment model is: modified fee for service, alternative payment model, or value-based purchasing. If it doesn’t lead to taking costs out of the system, it’s not sustainable. Period. We have to get at cost, and there are tens of millions of dollars of unnecessary costs and quality failures in our system due to uncontrolled clinical variation. You can’t get at those without clinician and physician engagement. That’s why if it’s leading to costs coming out, uncontrolled variation coming down, and quality improving, then I think the consolidation of hospital-based groups—emergency medicine being one of them—is a good thing.
Pages: 1 2 3 4 5 | Single Page





No Responses to “Emergency Medicine Leaders Discuss Drivers of Hospital Consolidation at ACEP15 Council Town Hall”