BA: Two basic questions from the hospital side are, is there an equity holder of the asset that is being acquired? Yes or no. The second is, is there a conversion of tax status? If the answer to either of those is yes, then you have to find a mechanism to purchase the equity from the entity that owns the asset. There is a community benefit typically that needs to be paid back going from a nonprofit to a for-profit tax status conversion. Nonprofit to nonprofit, which is the type of acquisition that we would be most engaged in at Mercy Health, is simply a member substitution with some commitment to that community for capital investment.
Explore This Issue
ACEP Now: Vol 35 – No 02 – February 2016RM: We’re not seeing just mergers and acquisitions; we saw a big wave of joint ventures. I’ve met with senior people at big for-profits who thought it was great, and now they seem to be falling apart. Is that a wave that’s coming and going? Is the joint venture idea of working with the hospital system on a downswing right now?
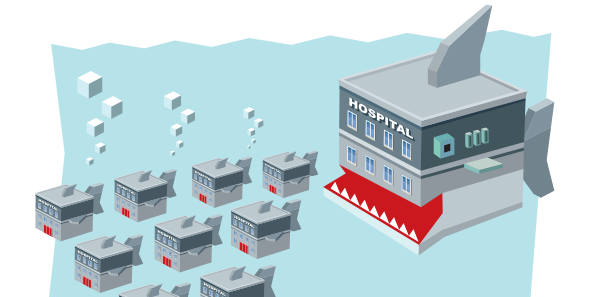
It’s just grow, grow, grow, and we can get another ounce of cost reduction out of our fixed infrastructure by adding the revenue of additional organizations. It is just about
balance sheet finances and operating infrastructure scale and leverage. —Brent Asplin, MD, MPH, FACEP
RI: We have a very large joint venture with HCA, and it’s healthy. We have a couple of other smaller ones. I don’t know if it’s going to take the country by storm, but I don’t think it’s going away.
JK: The issue comes back to physician control. It’s how much do we have to give up control over our own practice environment. I understand Brent’s perspective on decrease in variation. I think, with regard to joint ventures, the real issue is, if you’re going to joint venture with someone, how much control do you retain over your practice environment?
BA: Joint ventures are alive and well largely because of the moratorium on physician-owned hospitals. Obviously, the hottest space is around ambulatory surgery centers, but I’m sure there are quite a few joint venture models with freestanding emergency departments as well.
RM: One of the questions that comes up is, when these consolidations are done, do we see that, overall, physicians are harmed or benefited? I think there’s a lot of fear out there, which is why the question was asked.
I think when you talk about a merger, it’s much more about a partner. It’s more about who fits your philosophical approach to your organization, whether they’re going to bring value to you, and whether you’re going to bring value to them. —Savoy Brummer, MD, FACEP
SB: If you’re getting a huge windfall, you’re a single owner of a practice, and the lifespan of your clinical practice doesn’t extend outside of this windfall, then it could be largely beneficial. We’ve all had conversations as to what is the perceived value of your practice after you engage in some of these transactions. Many times, if you’re going to get a huge windfall up front, that means your clinical hourly is going to go down. Those are the rules of doing business.
Pages: 1 2 3 4 5 | Single Page





No Responses to “Emergency Medicine Leaders Discuss Mergers, Acquisitions at ACEP15 Council Town Hall”