Editor’s Note: The ACEP Council hosted a Town Hall meeting on mergers and acquisitions on Oct. 24, 2015, in Boston. Here is Part 2 of our edited transcript of the discussion.
Explore This Issue
ACEP Now: Vol 35 – No 02 – February 2016Introduction
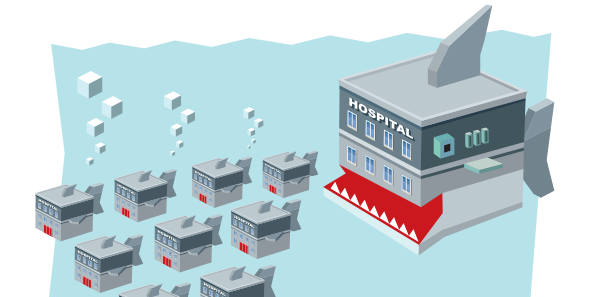
This is our Town Hall meeting and should represent a topic that is really important to the practice of emergency medicine, our specialty, and beyond: mergers and acquisitions. Many of us may not know a lot about this process and how it could impact us, but I think it’s time we discussed it so that we are all more informed about mergers and acquisitions in medicine. That’s why I titled this “Mergers and Acquisitions: The Medical Shark Tank.” I tried to get Mark Cuban; he still hasn’t responded to the request. I’ve asked Ricardo Martinez, who has a wealth of broad health care knowledge, to moderate this session.
—Kevin M. Klauer, DO, EJD, FACEP, ACEP Council Speaker (2013–2015), chief medical officer–emergency medicine and chief risk officer for TeamHealth, and ACEP Now medical editor-in-chief
Moderator

Ricardo Martinez, MD, FACEP, chief medical officer for North Highland Worldwide Consulting and assistant professor of emergency medicine at Emory University in Atlanta.
Participants

Brent Asplin, MD, MPH, FACEP, chief clinical officer for Mercy Health in Ohio
Savoy Brummer, MD, FACEP, vice president of practice development at CEP America in Belleville, Illinois, and chair of the ACEP Democratic Group Section
Ray Iannaccone, MD, FACEP, president of EmCare
Jay Kaplan, MD, FACEP, President of ACEP; director of the patient experience for CEP America in Emeryville, California; and a practicing clinician in the emergency department at Marin General Hospital in Greenbrae, California
RM: How are [emergency group] mergers funded?
RI: If your group is acquired, they’ll give you, in return for the group and the revenue stream that comes off of that, cash—which I think is the most common—stock, or both. For the company that’s buying it, they have cash they’re ready to pay you, or they borrow money from an institution to pay you, or in the case of stock, they’ll give you stock.
RM: They would have the money to invest as part of that company and then take the revenues as they come down the road.
RI: Right. Some people will want to sell part of the group. The classic private equity deal would be that the private equity firm would give you some of what might be 40 percent or 60 percent, and then in another three to five years, they decide whether they sell to somebody else or do an [initial public offering]. Doing that would be another opportunity for the owners of the group to get more money.
JK: I have a little bit of a bias here. I majored in social studies in college, and so I studied economics, history, and government. I personally would rather have health care dollars stay in the hands of those in health care. My personal preference, if I had a choice, would be to have an acquisition happen with organizations that have funds available and don’t have to go to a venture capital partner to get the funds. I think when you do that, you run the risk of losing control. In my experience, it’s much better to merge than it is to be acquired. Let me be clear that acquisitions can either be voluntary or involuntary. You can be told you must join that group, or you can do it on your own. I think if you can do it voluntarily, you’re in a much better position to negotiate and to get more than if you’re told you can’t continue the way you are and you have to be acquired by that group.
I think if you can do it voluntarily, you’re in a much better position to negotiate and to get more than if you’re told you can’t continue the way you are and you have to be acquired by that group. —Jay Kaplan, MD, FACEP
RI: I want to clarify for some folks that I think the situation Jay’s talking about is who’s telling you, “You have to be acquired.” It may be your hospital system, which will come to you and say, “Listen, we can’t do this with 23 different groups.”
SB: To follow up on what Jay had said, I think that all groups are at risk of being acquired. Whether your group is a single, independent practice or a large publicly held entity, you’re all at risk for being acquired by someone under some unforeseen circumstance. There are certain differences in how funding occurs. I know that most democratic groups are not looking at going to private equity markets to fund acquisitions. In fact, for the majority of my constituents and especially for my organization, we look at acquisitions as a needless activity, to some extent. Why would we invest $100–$200 million to acquire a group when we can do so organically and with same-store growth? Our philosophical approach has been that we don’t necessarily have to purchase the market to obtain a piece of that market. That’s a very different view of our growth strategy.
BA: Two basic questions from the hospital side are, is there an equity holder of the asset that is being acquired? Yes or no. The second is, is there a conversion of tax status? If the answer to either of those is yes, then you have to find a mechanism to purchase the equity from the entity that owns the asset. There is a community benefit typically that needs to be paid back going from a nonprofit to a for-profit tax status conversion. Nonprofit to nonprofit, which is the type of acquisition that we would be most engaged in at Mercy Health, is simply a member substitution with some commitment to that community for capital investment.
RM: We’re not seeing just mergers and acquisitions; we saw a big wave of joint ventures. I’ve met with senior people at big for-profits who thought it was great, and now they seem to be falling apart. Is that a wave that’s coming and going? Is the joint venture idea of working with the hospital system on a downswing right now?
It’s just grow, grow, grow, and we can get another ounce of cost reduction out of our fixed infrastructure by adding the revenue of additional organizations. It is just about
balance sheet finances and operating infrastructure scale and leverage. —Brent Asplin, MD, MPH, FACEP
RI: We have a very large joint venture with HCA, and it’s healthy. We have a couple of other smaller ones. I don’t know if it’s going to take the country by storm, but I don’t think it’s going away.
JK: The issue comes back to physician control. It’s how much do we have to give up control over our own practice environment. I understand Brent’s perspective on decrease in variation. I think, with regard to joint ventures, the real issue is, if you’re going to joint venture with someone, how much control do you retain over your practice environment?
BA: Joint ventures are alive and well largely because of the moratorium on physician-owned hospitals. Obviously, the hottest space is around ambulatory surgery centers, but I’m sure there are quite a few joint venture models with freestanding emergency departments as well.
RM: One of the questions that comes up is, when these consolidations are done, do we see that, overall, physicians are harmed or benefited? I think there’s a lot of fear out there, which is why the question was asked.
I think when you talk about a merger, it’s much more about a partner. It’s more about who fits your philosophical approach to your organization, whether they’re going to bring value to you, and whether you’re going to bring value to them. —Savoy Brummer, MD, FACEP
SB: If you’re getting a huge windfall, you’re a single owner of a practice, and the lifespan of your clinical practice doesn’t extend outside of this windfall, then it could be largely beneficial. We’ve all had conversations as to what is the perceived value of your practice after you engage in some of these transactions. Many times, if you’re going to get a huge windfall up front, that means your clinical hourly is going to go down. Those are the rules of doing business.
RI: If you’re looking at consolidating or merging or being acquired, you should be very careful with the partner that you pick. The point that Savoy made is important to keep in mind; there are physician-owned groups of all different kinds. As the former chair of the Democratic Group Practice Section, which Savoy is now the chair of, we struggled a lot, even internally, trying to define what a democratic physician group was. There is a large variety. Emergency Medical Associates, like CEP, is a very broadly owned group. There are other groups that are owned by one person. The impact of the sale of each of those groups is very different from the others. In EMA, we always had to take whatever number that somebody would be willing to offer and divide it by our number of partners. Years ago, when Jay was in the group, I think it was split by 60. A few years ago, when we talked about it, it was 200. This year, when we finally did it, I think it was 250. The payment looks big, but when you divide it by 250, nobody’s retiring. It’s not that kind of money. The reasons we did it has something more to do with that change. There was this equation that was always done, and it was never enough money to make it worthwhile for us to do it just for the money. This time, we decided to join EmCare, and there were other things that we talked about strategically that we felt were more important. If you’re one or two people and you own a contract with four or five hospitals, you’ll be offered a lot of money.
JK: Can I make two comments, Ricardo? Number one, it can benefit you if you have had a cantankerous relationship with your hospitalists and, all of a sudden, you and your hospitalists are part of the same group. We found that it really helps to facilitate communication and patient flow when you have the same ethos and culture among the emergency physicians and the hospitalists. The second is a little bit more conceptual. Do you want the doctors that you work with to feel like owners, or do you want them to feel like renters? There is a difference between an owner and a renter and between being a winner and a whiner. Whiners only complain about things; they come in, they do their hours, and then they leave. Winners take responsibility for issues. If a problem comes up, they’re going to fix it; they’re not going to run off and let somebody else fix it. However you accomplish this, whether you’re part of a large group or whether you’re part of a small group, we want our doctors to feel like owners. When many of us first went into practice, the model was that emergency physicians felt like cowboys. As cowboys, we come in, do our hours, and the rest of the time you spend on the beach, spend in the mountains trekking, or whatever else you’d like to do. That’s changed. Now, if we’re going to be successful as emergency physicians, we really have to become integral parts of the social fabric of our hospitals. The only way to do that is to make people feel like we’re owners in whatever model. If becoming a part of a large group through a merger or acquisition can help you feel more like you have a piece of the rock, fine. If it doesn’t and if it moves away from that, then ultimately it’s going to be harmful.
I don’t think it matters whether you’re the acquired or the acquirer. It’s about going into it with the willingness to have your culture change. Because no matter how similar you are, there are differences. —Ray Iannaccone, MD, FACEP
BA: I think these are great comments. I love the theme of ownership. There are large systems that are clearly just on a scale-and-leverage play. It’s just grow, grow, grow, and we can get another ounce of cost reduction out of our fixed infrastructure by adding the revenue of additional organizations. It is just about balance sheet finances and operating infrastructure scale and leverage. I don’t think they’re ultimately going to win because if you stretch that out between states and become these giant organizations on the hospital side, it’s really going to be difficult without engaging physicians as operators in clinical redesign. That is where the next huge treasure trove of cost reduction is in hospital operations in this country, and it’s going to result in much better outcomes. You can’t get that without engagement and ownership of physicians and their leadership, whether they’re part of your system from an employment standpoint or contractual relationship. That’s what we’re striving for. It’s a journey; we’re not there yet, but that is the model that will beat consolidation and growth for scale and leverage at all cost.
RM: I like that a lot. Culture eats strategy for lunch, so I’m really interested in this theme. You talked about engagement. What are some of the big ways to address making it work, and what are some of the big pitfalls in implementing mergers and acquisitions?
SB: I would tend to agree with Jay. I think mergers and acquisitions are actually two separate types of categories. Philosophically, an acquisition is much more of a transactional arrangement. I think when you talk about a merger, it’s much more about a partner. It’s more about who fits your philosophical approach to your organization, whether they’re going to bring value to you, and whether you’re going to bring value to them. Especially with democratic groups, they come frequently to CEP America, and they ask about our structure and our approach. Sometimes it works out, and sometimes it doesn’t, but the time and energy it takes is much more than a profit-loss margin type of discussion and, instead, more of a cultural empowerment professionalism type of discussion.
RM: I do want to make a comment on that. Do you remember Daimler and Chrysler merging years ago? The joke was, “How to do you pronounce Daimler-Chrysler? The Chrysler’s silent.” That thing fell apart because of culture.
RI: That’s the conventional wisdom, and it’s my experience also that mergers or acquisitions fail because of different cultures. I don’t think it matters whether it’s a merger or an acquisition. I don’t think it matters whether you’re the acquired or the acquirer. It’s about going into it with the willingness to have your culture change. Because no matter how similar you are, there are differences. There can’t be a need or an expectation that everything’s going to stay the same after the transaction.
Council Town Hall highlights will continue in the March issue.





No Responses to “Emergency Medicine Leaders Discuss Mergers, Acquisitions at ACEP15 Council Town Hall”